Corneal imaging has become increasingly important to clinical practice for everyone from the primary eye care provider to the tertiary care corneal and refractive specialist. I have endeavored in this article to briefly touch upon the existing technology and what’s on the horizon. For reasons of space, it is not possible to extensively review all currently available devices, so select examples have been mentioned in each category.
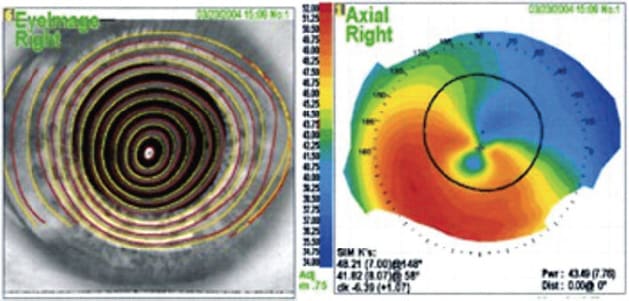
Corneal topography (CT) first appeared in the early ’80s when Steve Klyce and others began to analyze concentric ring images (Placido discs) with computers, generating color-coded curvature maps. CT by anterior surface reflectance remains today the most sensitive method of detecting curvature and elevation of the anterior corneal surface. Most clinicians make the mistake of thinking that CT measures the anterior corneal surface, but academicians and topography gurus remind us that the reflection actually derives from the tear film coating the corneal epithelium. This allows Placido imaging to also inform about integrity and continuity of the tear film, which is important in evaluation for ocular surface disease and any elective corneal refractive or IOL care.
CT became popular in the ’80s and ’90s as a quick, efficient method to identify normal and abnormal conditions of the eye, particularly keratoconus (KC). It became widely used in evaluating candidates for contact lens fitting, custom rigid gas permeable fitting, IOL care, and keratorefractive surgery, including LASIK and PRK. Indices arising from topography include Kmax (maximum steepness), topographic asymmetry, Klyce statistics and many others.
Like almost all “legacy” ophthalmic diagnostic devices, most corneal imaging systems evolved and exist today as variations on a theme of dedicated illumination systems (Placido discs or other patterns) combined with image sensors, attached to dedicated personal computers running proprietary software. These instruments typically sit on motorized tables in special testing rooms outside the normal exam lanes where basic testing, including refraction, slit lamp exam and tonometry is performed.
There are several portable, handheld topography systems (Oculus Easygraph, Keratron Piccolo [Optikon], Keratron Scout [Optikon], EyeSys Vista, and others), but these all lack the z-axis positional accuracy of larger systems and have failed to gain popularity. Cost for a single-purpose corneal topography instrument can vary from ~$8K on the low end to near $20K on the high end.
Non-Placido Instruments
Patterns other than Placido discs can be used to measure curvature and optical properties of the corneal front surface. A grid pattern is used by both the iDesign Refractive Studio (Johnson & Johnson Vision) and the Cassini topographer (i-Optics). These eliminate some possible errors that can occur during curvature reconstruction in Placido systems.
Dual-Surface Imaging Devices
Dual-surface imaging devices first appeared in the late ’90s. These combine anterior surface imaging, posterior surface imaging and full-surface thickness mapping capability. Posterior surface imaging by tomography, first using slit-scan imaging in the Orbscan (Orbtek, subsequently acquired by Bausch & Lomb), then Scheimpflug imaging, as in the Pentacam (Oculus) and Galilei (Ziemer Ophthalmic Systems), has certainly augmented our ability to recognize early pathology. This testing is now considered standard of care before laser refractive surgery, and many surgeons routinely perform this testing as a part of premium IOL care. Dual-surface imaging allows one to recognize anterior steepening, topographic asymmetry, abnormal posterior surface bulge, and decentration of the point of minimum thickness, which are all indicative of potential pathology, and all of which increase index of suspicion for LASIK candidacy, among other things.
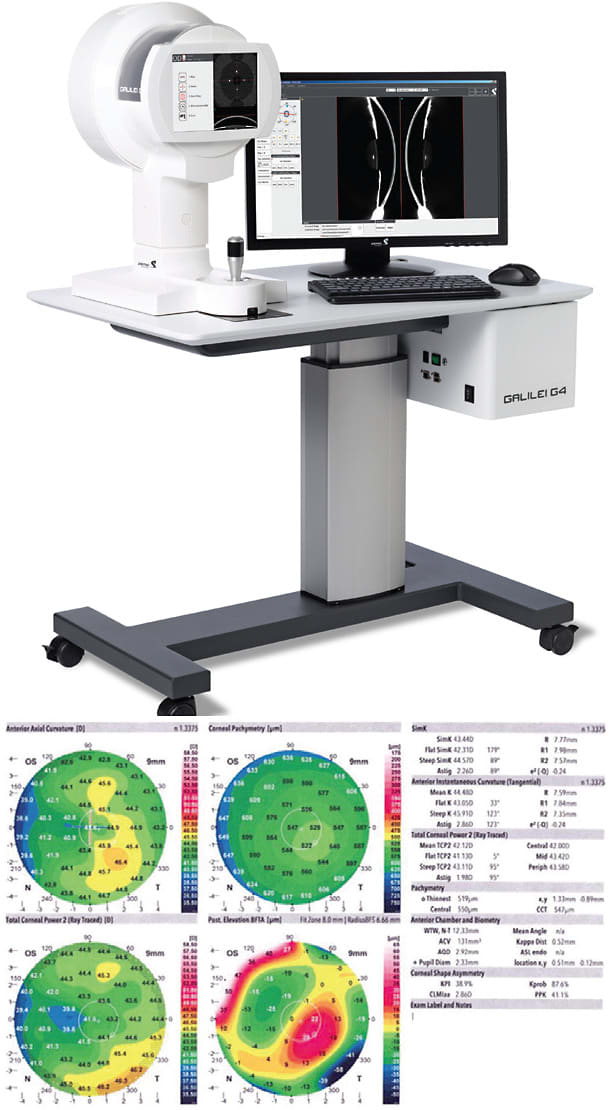
Posterior surface imaging and thickness mapping provide additional frames of reference, allowing identification of certain pathology states. Abnormal elevation, as seen on a posterior float map, can help identify forceful eye rubbing and KC, for example. Abnormalities on a thickness map can include reduced central corneal thickness (CCT) and decentration of the point of minimum thickness (away from the geometric center), typically down and nasal in KC.
Cost for dual-surface imaging devices is amusingly referred to by refractive surgeons as the “refractive surgery nickel”–around $50K.

CORNEAL TOPOGRAPHY SYSTEM IN THE PIPELINE
Advances in mobile computing and imaging technology now enable topography (and conceivably tomography, among other ophthalmic diagnostics) to be done on a modern smartphone, rather than a desktop computer. In addition, the entire field of computational photography has evolved over the past ~15 years to vastly enhance image detection and processing.
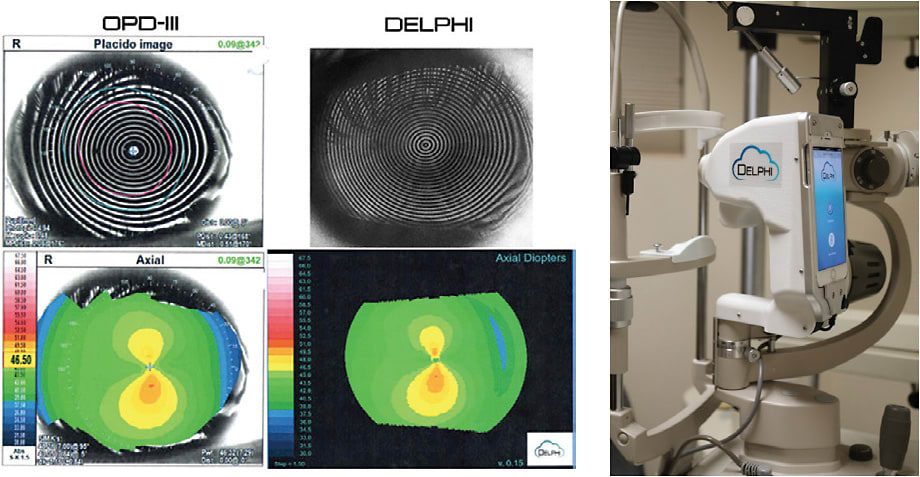
This constellation of factors, in part, inspired me to begin development of an ultra-low-cost corneal topography system about 5 years ago. The Delphi topography system has imaging optics and a Placido illumination system attached to a dedicated smartphone. The unit mounts on any slit-lamp, using the universal positioning hole at the pivot-point of the slit beam and microscope. A unique auto-capture system engenders exceptional ease of use. Data is uploaded and stored in cloud servers enabling “big data” analytics and artificial intelligence (“AI”) to enhance diagnostic accuracy and therapeutic guidance. This kind of real-time expert analysis should eliminate ambiguity for the general eye care provider: Imagine having input from the world’s best topography experts available as you review each study.
The Delphi will offer Placido topography, pupillometry and corneal ray tracing functionality. Our prototype system shows +/- 25 μ z-axis positional accuracy; better than any existing commercial system. It is capable of better central data capture than any current commercial topography system, as the central ring subtends only 240 μ on a 44 D cornea. Maps will be rendered virtually instantly on the smartphone display, and the cloud portal will enable different map scales, map types, overlays, etc. A significant value-add will be the ability to offer cloud-based difference mapping (running in the background, alerting the provider only if change is identified).
This system is envisioned as an ultra-low-cost platform enabling broad-based topography screening, potentially with every routine annual eye exam and contact lens-fitting visit. Low provider cost is critical for corneal topography to become standard of care.
The Delphi is anticipated to cost roughly $2K to place, plus a monthly software-as-a-service (“SaaS”) fee in the range of $120.
Machine intelligence that can inform diagnostics has existed for decades. The earliest corneal topography devices employed neural networks, which are fixed databases of relatively small size. These served a purpose for over 25 years in establishing baseline references, KC indices, and many other indicators of corneal curvature normality or abnormality. The ability to aggregate studies in a cloud server environment enables databases three to five orders of magnitude larger than those used in any neural net context, which should improve accuracy, specificity and provide excellent population-based statistical references.
It is hoped that funding can be secured to complete development. The COVID-19 pandemic has interposed certain industry pull-back affecting this project and many others, but I remain optimistic that we’ll be able to deliver a product to market within a reasonable time frame. One truth about both technology development and refractive surgery is that one should never over-promise and under-deliver, so I’m kind of sticking my neck out to write about this before securing a pathway to commercial release.
There exists an opportunity for a low-cost topography system with high sensitivity and accuracy, that can be broadly deployed and used as a screening device for all new patients, annual exams, soft contact lens evaluations, etc. Early diagnosis of KC will be enhanced and facilitated by such technology. If successful, this platform can be used to offer other ophthalmic diagnostics with the same form factor, low cost, ease of use, etc. In theory, the future is bright; the devil is in the details!
High-Frequency, Digitally Enhanced Ultrasound
High-frequency, digitally enhanced ultrasound systems (Artemis, ArcScan, Inc.) taught the importance of epithelial thickness mapping (ETM) and its role in refractive surgery, but these single-purpose instruments were unfortunately too costly to be adopted by all but a select few refractive practices, as they run in the ~1.5 “nickel” range. ETM is informative in treating certain special situations and helps us understand the refractive contribution of epithelium when unusually thick or thin, as can be seen sometimes when evaluating patients who have unexpected refractive change after prior LASIK or SMILE. Swept-source OCT can also measure epithelial thickness and corneal thickness, as well as curvature of both surfaces.
OCT
OCT first gained broad popularity for macular and retinal nerve fiber layer imaging. As systems evolved, it became possible to incorporate corneal and anterior chamber angle imaging.
OCT can measure curvature and thickness, and can visualize pathology at a cellular level, such as epithelial ingrowth and false-plane dissection, as can occur in SMILE on rare ocassion. But it is not routinely used to generate the color maps of corneal curvature or elevation that are customarily generated by topography and tomography systems. Cost for a decent OCT system capable of ETM, such as the Avanti (Optovue), is in the two to three “refractive surgery nickel” range.

Single-purpose Wavefront Analysis Systems
Single-purpose wavefront analysis systems have also evolved over the past 20 years, and are now recognized as integral to optical system analysis, troubleshooting visual complaints, and advanced refractive surgery planning. All systems that measure higher-order aberrations also measure low-order, so provide autorefraction. Numerous wavefront-sensing instruments exist, some that are designed only to work within the framework of a larger package intended for laser refractive surgery, such as the iDesign Refractive Studio (Johnson & Johnson Vision), Alcon Wavelight Topolyzer, and Schwind wavefront systems. Popular stand-alone systems include the Zeiss Wasca and others. Visionix now offers a system with Placido anterior topography, Scheimpflug tomography and Shack-Hartmann aberrometry. These systems will set you back one or two “nickels.”

Combination Devices
Some of these are able to perform ray tracing, which adds wavefront analysis capability. The Nidek OPD-Scan-III is a very popular combo system offering topography, autorefraction and corneal aberrometry capability. This unit sells in the ~$40K range. The iTrace (Tracey Technologies) is also a topography + aberrometry system.

Confocal Microscopy
Confocal Microscopy enables assessment of the five corneal layers via illumination and high magnification. These features make them ideal for endothelial cell counts, studying corneal depth, corneal nerve morphology, and in diagnosing infectious keratitis. Examples include the CellCheck (Konan Medical) and Stellaris (Leica Microsystems). The latter is a research tool that will run in the range of four “nickels.”

Expansion
As our diagnostic sensitivity and therapeutic capabilities have expanded dramatically over the past 3 decades, the number and type of corneal imaging systems have expanded as well. The normal cornea is transparent, and used to be largely ignored by examiners looking into the eyes of patients. We are now well-served by a wide array of modern corneal imaging instruments that allow us to recognize the subtle nuances of microanatomy, structure, function, and optical contribution of this small bit of curved tissue that accounts for roughly two-thirds of the overall refractive power of the human eye. CP









