Be Mindful of Patient Selection
Proper patient selection is important for successful FLEK procedures. Ocular conditions, such as small orbits, narrow palpebral fissures and elevated glaucoma implants or blebs, that would prevent successful docking, should be avoided.
Caution should be taken with recent corneal or globe trauma and dense corneal scars or neovascularization that could prevent laser penetration (which requires a clear media), and interfere with trephination.
Additionally, patients should be able to lay flat and still during the procedure, so in select cases, such as where dementia, nystagmus, anxiety, or claustrophobia are present, and even in children, general anesthesia should be considered. (Topical, retrobulbar, systemic, and “verbal” anesthesia can help with comfort.)
FLEK can be performed in the pediatric population11, and it may have the added benefit of decreasing the risk of amblyopia.
Choose the Correct Trephination Pattern
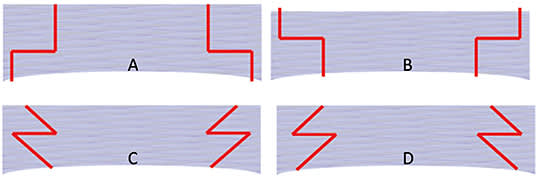
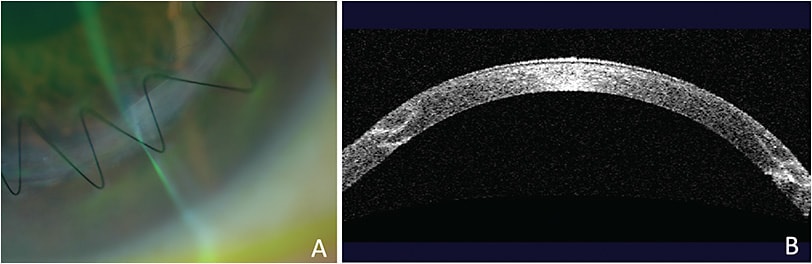
Numerous patterns of trephination have been described, including “top-hat,” “mushroom,” “zig-zag,” and “Christmas tree” patterns (Figure 1).
Be Mindful of Patient Selection
The “top-hat” design (larger diameter cut, posteriorly) has a large internal flange to help seal wounds, and transplants more endothelial cells, which is considered advantageous in conditions in which the endothelial layer is diseased, as in Fuchs’ endothelial dystrophy.
The “mushroom” pattern (larger diameter, cut anteriorly) replaces anterior stromal tissue, which is beneficial in anterior corneal pathologies, such as in keratoconus or anterior scars.
The “Christmas tree” and “zig-zag” trephination have angled side-cuts that help with tissue alignment, centration, and graft host apposition (Figure 2). These patterns allow for simple suturing through easily visualized lamellar tissue on the host and graft cornea, whereas the other patterns require more precise suture passes to evenly distribute corneal tissue. (In our practice, the “zig-zag” pattern is our preference, and it is used almost exclusively.)
The donor corneal tissue can be precut by the eye bank if one of the above patterns is desired. If the eye bank is unable to precut the tissue, the surgeon can cut the tissue using an artificial anterior chamber, making sure to use the same pattern, and cut parameters used to trephine the patient’s cornea. With the “zig-zag,” pattern, we typically cut the graft and host to the same size, however the graft can be undersized by 0.5 mm if the pre-operative keratometry readings are steep (i.e., keratoconus). In general, we leave a posterior layer of 70 μm of uncut tissue (as determined by a pachymetric map), as the femtosecond laser creates the laser cut trephination. Keeping the posterior stroma intact allows for a safe transit between the laser suite and the operating suite.
In addition to trephinating host corneal tissue, the femtosecond case can also place radial marks on the host cornea to help guide suture placement, and tissue distribution.
Once the host trephination is complete, the corneal button can be bluntly dissected to reveal the laser incisions. The anterior chamber is then entered with a blade, filled with viscoelastic material, and corneal scissors are used to cut along the defined plane. The donor cornea is then sutured onto the host with careful alignment and equal tissue distribution.8 (See “Other Uses for Femtosecond Laser,” below.)
Postoperative Management
Postoperative management of FLEK is similar to conventional keratoplasty, except that suture removal could be timed earlier, as the wound tends to be more stable. The dovetail graft-host junction, with an increased surface area for the donor and host corneal stroma adherence, offers a more stable wound, and, thus, allows for earlier removal of the suture and, in turn, more rapid recovery toward optimized vision. A similar course of topical antibiotics and corticosteroids are employed for these patients. These corneas typically have a smoother anterior curvature with lower levels of astigmatism.12-13
Employing FLEK
While traditional PK is an excellent procedure with great outcomes, FLEK continues to prove to be advantageous through the creation of a variety of trephination patterns that align the donor and host tissue for ultimate stability. The adaptation of femtosecond laser to keratoplasty surgery has allowed precise trephination patterns, strong wound integrity and apposition, and better visual outcomes with less astigmatism.
OTHER USES FOR FEMTOSECOND LASER
In addition to a full-thickness corneal transplant, the femtosecond laser can be used for lamellar keratoplasty: deep anterior lamellar keratoplasty (DALK), anterior lamellar keratoplasty (ALK), Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemet’s membrane endothelial keratoplasty (DMEK).
During DALK, a plane is made 50 μm to 100 μm anterior to the endothelium, and this is the starting point for big-bubble dissection. In the event of Descemet’s rupture during dissection, conversion to a full thickness transplant can be done, while maintaining the benefits of the femtosecond laser incision.14-15 (During DSAEK, the trephine is programed to cut 120 μm to 150 μm of lenticule tissue with corresponding host depth.16
During DMEK, a descemetorhexis is created with depth that extends from 100 μm above the thinnest measured corneal depth to 100 μm below the thinnest measured corneal depth.12
Femto-DSAEK procedures have better centration, thin-ner tissue cuts, and earlier corneal detergecense.16 These procedures are found to have decreased risk of postoperative detachment,17 re-bubble rates,17 and endothelial cell loss.17,18 Femto-DALK procedures are found to have improved visual outcomes, earlier suture removal 19, 20, and increased wound healing.
Something else to consider: FLEK lasers can also be used for refractive surgery, astigmatic incisions, corneal inlays, and intrastromal corneal ring segments, which can offset their cost. Also, new codes to help with the cost can be added on to the primary keratoplasty procedure performed. Code +0298T is used when corneal incisions in the donor cornea are created using a laser, and +0290T is used when corneal incisions in the recipient cornea are created using a laser, both in preparation for penetrating or lamellar keratoplasty. A caveat: There is an increase in surgery time when performing femtosecond cuts on donor and host tissue. CP
References:
- Steinert RF, Ignacio TS, Sarayba MA. “Top-hat”-shaped penetrating keratoplasty using the femtosecond laser. Am J Ophthalmol. 2007;143(4):689-691.
- Farid M, Kim M, Steinert RF. Results of penetrating keratoplasty performed with a femtosecond laser zigzag incision: initial report. Ophthalmology. 2007;114(12):2208-2212.
- Farid M, Steinert RF, Gaster RN, Winston C, Lin A. Comparison of penetrating keratoplasty performed with a femtosecond laser zig-zag incision versus conventional blade trephination. Ophthalmology. 2009;116(9):1638-1643.
- Buratto L, Böhm E. The use of the femtosecond laser in penetrating keratoplasty. Am J Ophthalmol. 2007;143(5):737-742.
- Price FW Jr, Price MO. Femtosecond laser shaped penetrating keratoplasty: one-year results utilizing a top-hat configuration. Am J Ophthalmol. 2008;145(2):210-214.
- Cheng YY, Tahzib NG, van Rij G, et al. Femtosecond laser-assisted inverted mushroom keratoplasty. Cornea. 2008;27(6):679-685.
- Bahar I, Kaiserman I, Lange AP, et al. Femtosecond laser versus manual dissection for top hat penetrating keratoplasty. Br J Ophthalmol. 2009;93(1):73-78.
- Heur M, Tang M, Yiu S, Zhang X, Huang D. Investigation of femtosecond laser-enabled keratoplasty wound geometry using optical coherence tomography. Cornea. 2011;30(8):889-894.
- Wade M, Muniz Castro H, Garg S, et al. Long-Term Results of Femtosecond Laser-Enabled Keratoplasty With Zig-Zag Trephination. Cornea. 2019;38(1):42-49.
- Chamberlain W, Omid N, Lin A, Farid M, Gaster RN, Steinert RF. Comparison of corneal surface higher-order aberrations after endothelial keratoplasty, femtosecond laser-assisted keratoplasty, and conventional penetrating keratoplasty. Cornea. 2012;31(1):6-13.
- Elkamshoushy A, Gonnah R, Madi S, Beltz J. Single-piece femtosecond-assisted mushroom keratoplasty in children. J AAPOS. 2019;23(1):28.e1-28.e5
- Chamberlain WD, Rush SW, Mathers WD, Cabezas M, Fraunfelder FW. Comparison of femtosecond laser-assisted keratoplasty versus conventional penetrating keratoplasty. Ophthalmology. 2011;118(3):486-491.
- Gaster RN, Dumitrascu O, Rabinowitz YS. Penetrating keratoplasty using femtosecond laser-enabled keratoplasty with zig-zag incisions versus a mechanical trephine in patients with keratoconus. Br J Ophthalmol. 2012;96(9):1195-1199.
- Price FW Jr, Price MO, Grandin JC, Kwon R. Deep anterior lamellar keratoplasty with femtosecond-laser zigzag incisions. J Cataract Refract Surg. 2009;35(5):804-808.
- Buzzonetti L, Laborante A, Petrocelli G. Standardized big-bubble technique in deep anterior lamellar keratoplasty assisted by the femtosecond laser. J Cataract Refract Surg. 2010;36(10):1631-1636.
- Hosny MH, Marrie A, Karim Sidky M, GamalEldin S, Salem M. Results of Femtosecond Laser-Assisted Descemet Stripping Automated Endothelial Keratoplasty. J Ophthalmol. 2017;2017:8984367.
- Sorkin N, Mednick Z, Einan-Lifshitz A, et al. Three-Year Outcome Comparison Between Femtosecond Laser-Assisted and Manual Descemet Membrane Endothelial Keratoplasty. Cornea. 2019;38(7):812-816.
- Chen H, Tian L, Le Q, et al. Femtosecond laser-assisted Descemet’s stripping endothelial keratoplasty: a prospective study of 6-month visual outcomes, corneal thickness and endothelial cell loss. Int Ophthalmol. 2020;40(8):2065-2075.
- Salouti R., Zamani, M, Ghoreyshi M, Dapena I, Melles GRJ, and Nowroozzadeh MH, Comparison between manual trephination versus femtosecond laser-assisted deep anterior lamellar keratoplasty for keratoconus. Br J Ophthalmol. 2019;103(12):1716-1723.
- Blériot A, Maryin E, Lebranchu P, et al. Comparison of 12-month anatomic and functional results between Z6 femtosecond laser-assisted and manual trephination in deep anterior lamellar keratoplasty for advanced keratoconus. J. Fr. Ophtalmol. 2017;40(6):e193-e200.