Deep anterior lamellar keratoplasty (DALK) has the advantage of preservation of recipient endothelium and Descemet’s membrane (DM), limited interface scarring, low intraoperative and postoperative complications, as well as a track record of reproducible success. Therefore, it is favored for the surgical treatment of corneal ectatic disorders, including keratoconus, pellucid marginal degeneration, and iatrogenic corneal ectasia induced by refractive surgery in which the endothelial layer is normal, and only the stromal layers are diseased.1-5
While DALK can be performed using a variety of techniques, this article will focus on Anwar’s big-bubble technique, referred to here as big-bubble keratoplasty (BBK) (Figure 1). The technique has a long track record of success, a large amount of long-term peer-reviewed literature, and, based on my experience, has the widest adoption worldwide of the various techniques. The comparison of BBK with PK is summarized as follows:
- BBK is equivalent to PK in recovery of best spectacle-corrected visual acuity, particularly if minimal residual host stromal thickness is retained.6
- BBK is superior to PK for preservation of endothelial cell density.6-8
- Long-term endothelial cell loss in BBK was moderate and lower than PK grafts.7 In fact, endothelial immune graft rejection cannot occur after DALK.
- Suture-related complications are decreased because sutures can often be removed earlier in BBK cases.
- BBK has a significantly lower incidence of choroidal hemorrhage versus PK, with a virtually impossible risk of expulsive choroidal hemorrhage, given its extraocular nature.
- Anecdotal reports have described increased resistance of BBK grafts to a rupture of the globe following blunt trauma.9

Surgical Technique
BBK begins with donor tissue preparation, as in the case of PK, with full-thickness trephination of the donor cornea (diameters typically range from 7.0 mm to 9.0 mm) using the surgeon’s desired trephine punch system.
The host cornea is then trephined to a depth that does not risk trephining through the DM, sometimes just to a 300 μm or 350 μm depth, depending on pre-operative pachymetry of the thinnest quadrant of the cornea at the mid periphery. Trephine systems that allow for titrated trephination and are on a vacuum can be helpful in avoiding full-thickness trephination. The donor button may be slightly larger than the recipient bed (typically 0.25 mm) or the same size, depending on the corneal pathology. As in PK done in ectatic eyes, the typical approach is to perform same-size trephinations on ectatic corneas to flatten the corneal curvature.
Pneumodissection of the DM away from the posterior stroma is the goal of creating a “big bubble.” My approach is to attach a 27-gauge or 30-gauge cannula firmly to an air-filled syringe with the tip bent to a 30° to 40° angle 5 mm away from the tip edge.
The tip is inserted bevel-down deep into the trephination groove, and advanced further into the stroma and parallel to the posterior corneal surface. There is risk of puncture through the DM when using a needle for this step of the surgery, especially as visualization of the depth of penetration is challenging with a surgical microscope. Some surgeons prefer to make a small lamellar pocket beginning in the trephination groove, using instruments specifically developed for DALK. The thought is to create a tunnel in the posterior stroma to facilitate passing a 27-gauge or 30-gauge cannula attached to a syringe of air toward the pupil. Using DALK-specific instruments may help lessen the slightly higher risk of perforation into the chamber with a needle.
Once the tip of the needle or cannula on a syringe filled with air is well buried into the corneal stroma with a 3 mm to 4 mm advancement from the trephination groove, the surgeon injects air using a moderate amount of force. The stroma becomes opaque as the air advances away from the tip, causing crepitus in the stromal layers. If the air injection is at a depth close to the deep stroma, the leading edge of the crepitus reaches the potential space between the DM and the posterior stroma, and dissects the DM away with an expanded “big bubble.” Once the border of the big bubble reaches the trephination area, injection ceases.
With a proper big-bubble formation, the eye pressure becomes firm. In fact, if the eye pressure remains normal by palpation after air bubble injection, the big bubble likely did not induce a DM detachment. Should this be the case, the needle or cannula can be inserted into a different area with the process repeated until it is apparent that the big bubble formed, and the DM detached.
A caveat: Corneal ectatic disorders with previous corneal hydrops should undergo PK and not BBK, as the air injection step in the latter will force the previous DM to tear open and allow air to escape into the anterior chamber. That said, experienced DALK surgeons have reported completion of DALK using a manual layer-by-layer dissection, even in the setting of a previous DM tear.10
Once the big bubble is formed and the DM detached in BBK, a keratectomy (bulk keratectomy) is then performed with a crescent blade removing 50% of stromal tissue anterior to the bubble (Figure 2), followed by a limbal paracentesis to lower IOP. The bulk keratectomy step allows for better visualization through the emphysematous, cloudy cornea. Unal et al described a modified version of BBK in which the bulk keratectomy is performed first after the recipient trephination step.11 Once completed, the cannula/needle is inserted to create the big bubble. This technique is felt to provide better visualization of the big bubble creation, as the stromal layer has been significantly thinned from the bulk keratectomy.11 If I do not get a big bubble initially, I create the bulk keratectomy and then attempt the big bubble a second time, so I have two chances (before and after the bulk keratectomy).
After creation of the paracentesis, there is a significant IOP reduction within the anterior chamber. At this point, a small air bubble can be injected into the anterior chamber to confirm the presence of the big bubble.12,13 If the small bubble remains in the periphery, the DM has detached appropriately. If the small bubble floats centrally and becomes invisible from the central emphysematous cornea, the big bubble has not been created, and the DM is not detached. In this case, the air injection step should be performed with the insertion of the needle or cannula initiated through an area of the trephination with the least amount of opacity to allow for visualization.
Once the big bubble is confirmed, a sharp blade is then inserted into the stroma toward the air bubble and quickly withdrawn, so that a perforation in the DM does not occur as the air bubble collapses. Placing a drop of viscoelastic over the central stroma prior to blade insertion can decrease the speed of air bubble release, and lessen the risk of perforation of the blade through DM. Without the viscoelastic step, air escape can be so rapid that DM perforation can occur prior to the fast withdrawal of the sharp blade. If the stromal opening made with the blade is too small, it is difficult to find the entry site for dissecting spatulas, making it arduous to separate stroma and DM.
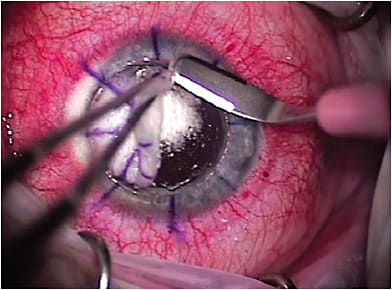
A plane is then created between the stroma and DM by injecting cohesive viscoelastic through the stromal opening whilst expressing more acqeous from the paracentesis to allow for the big bubble to expand and push the DM away from the stroma and risk of rupture. Blunt dissecting spatulas are then used to gently dissect any stromal adhesions to the DM all the way to the trephination. The corneal stroma is removed completely within the trephination circle, using curved scissors ideally with rounded tips. The stroma can be cut in quadrants for careful removal, with the goal of leaving an intact DM layer (Figure 3). DM is peeled from the donor cornea (azo dye can facilitate visualization during DM removal), and the corneal tissue then is secured to the host tissue using a 10-0 nylon suture. Expert surgeons with reliable and high rates of success in achieving the big-bubble separation or being able to continue with DALK, even when the DM is ruptured, can request a donor cornea suitable only for anterior lamellar keratoplasty. Most surgeons, though, request a PK cornea, should an intraoperative macro perforation and conversion to PK be needed.

The main considerations when converting from BBK to PK include poor visualization through an emphysematous white cornea, avoiding retained DM, keeping within the trephined margins of the opaque cornea, prevention of iatrogenic iridectomies, and avoidance of lens capsule trauma.14,15 Viscoelastic instillation in the anterior chamber can be useful to tamponade the iris and prevent iatrogenic iridectomy formation, and trypan blue dye can facilitate easier identification of recipient DM, so retained fragments are not left behind.15
Complications
Complications of BBK fall under intraoperative and postoperative:
• Intra-operative complications. These may include donor-recipient mismatch of tissue and inadequate suture tension; perforation of DM6 and failure to create the big bubble.3
Donor-recipient mismatch can be avoided if the donor tissue is oversized by 0.25 mm. Some surgeons prefer to have the donor and recipient trephination sizes the same in keracotonus to reduce the risk of myopia postoperatively. In these cases, suture tension often needs to be tighter than in PK to reduce the risk of early graft dehiscence. In such circumstances, interrupted sutures may provide an advantage over running sutures to provide better wound integrity. Mismatch may also occur with the donor graft thickness far exceeding the recipient’s thin ectatic peripheral cornea, leading to an elevated edge of the donor cornea at the graft-host junction. This mismatch may be more challenging and if it occurs, suture removal needs to be performed in very late stages to reduce the risk of graft dehiscence.
If the first attempt at big-bubble formation fails, the needle or cannula should be reinserted in a different position within the trephined interface with multiple attempts until the bubble formation occurs. In cases in which a big bubble cannot be created, a layer-to-layer dissection must be weighed versus conversion to PK.
Microperforations can often be saved with hydration of the remaining stromal tissue or by leaving residual stroma in the region of perforation. Additionally, the anterior chamber should be filled with air at the completion of the case to prevent a double anterior chamber.16 (Figure 4). In this case, air bubble management becomes critical to avoid a pupillary block induced by the air bubble. Cycloplegic agents, topical ocular hypotensive agents, and/or oral diuretics, such as acetazolamide, can be helpful in preventing pupillary block if a significant amount of air must be left in the anterior chamber. A small inferior peripheral iridectomy may also be helpful to protect against pupillary block.

In cases of macroperforation and conversion to PK, the donor corneal button can quickly become utilized for PK without the loss of donor endothelium. The trephined groove can easily be followed with curved corneal scissors to excise the entire tissue within the trephined zone.
• Postoperative complications. These include post-keratoplasty astigmatism, potential interface complications (i.e., interface haze, interface infectious keratitis, scarring, debris, epithelial ingrowth, DM wrinkles, interface heme, and double anterior chamber) and stromal graft rejection.
To overcome the suture-related complications of astigmatism, BBK allows for early suture removal, as the graft-host healing is more stable, given the intact DM. Removing sutures sooner allows for quicker refractive stability, and less risk of suture-related erosions or infections compared to full-thickness grafts. That said, careful consideration must always be given here, as anecdotal reports have demonstrated that spontaneous wound dehiscence can occur with DALK as with PK.17,18
Residual host stromal tissue is the typical cause of interface haze and scarring, as complete Descemet’s baring surgery avoids interface haze/scars. The majority of published literature on BBK suggests interface haze decreases with time, and is rarely visually significant long-term in both clinical and confocal microscopy studies.2,5,19,20
Interface infectious keratitis can occur, albeit rarely, from the donor cornea or represent an infection from flora on the ocular surface of the recipient. These cases need to have a culture if possible. If the infection is too deep for culture, a braided vicryl suture can be passed through the interface infiltrate from the corneal surface, and the braid will collect the infectious agent, and the suture can be sent for culture. Confocal microscopy may be helpful in some infections. Treatment needs to be aimed at treating the identified organism topically and orally. Graft replacement may be needed or conversion to PK if the infection enters the anterior chamber. Intracameral and subconjunctival anti-infection medicines can be administered at the time of repeat surgery.
Finally, stromal graft rejection episodes are responsive to corticosteroids, and can often be reversed without need for repeat grafting.
BBK’s Value
The published literature demonstrates BBK affords equivalent vision to patients undergoing PK surgery, allows for minimized suture-related complications, avoidance of an open sky procedure and elimination of endothelial graft rejection. In addition, anecdotal reports suggest BBK carries a theoretical advantage of increased tectonic support compared to PK. As a result, anterior segment surgeons should consider adopting this surgical technique over PK for any corneal ectatic disorder patient needing keratoplasty surgery after failure of conservative treatment. CP
References
- Amayem AF, Anwar M. Fluid lamellar keratoplasty in keratoconus. Ophthalmology. 2000;107(1):76-79.
- Anwar M, Teichmann KD. Big-bubble technique to bare Descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28(3):398-403.
- Anwar M, Teichmann KD. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet’s membrane. Cornea. 2002;21(4):374-383.
- Shimazaki J, Shimmura S, Ishioka M, Tsubota K. Randomized clinical trial of deep lamellar keratoplasty vs penetrating keratoplasty. Am J Ophthalmol. 2002;134(2):159-165.
- Fogla R, Padmanabhan P. Results of deep lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2006;141(2):254-259.
- Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(1):209-218.
- Kubaloglu A, Sari ES, Unal M, et al. Long-term results of deep anterior lamellar keratoplasty for the treatment of keratoconus. Am J Ophthalmol. 2011;151(5):760-767.
- Cheng YY, Visser N, Schouten JS, et al. Endothelial cell loss and visual outcome of deep anterior lamellar keratoplasty versus penetrating keratoplasty: a randomized multicenter clinical trial. Ophthalmology. 2011;118(2):302-329.
- Lee WB, Mathys KC. Traumatic wound dehiscence after DALK. J Cataract Refract Surg. 2009;35(6):1129-1131.
- Chew ACY, Mehta JS, Tan DTH. Deep anterior lamellar keratoplasty after resolution of hydrops in keratoconus. Cornea. 2011;30(4):454-459.
- Unal M, Bilgin B, Yucel I, Akar Y, Apaydin C. Conversion to deep anterior lamellar keratoplasty (DALK): learning curve with big-bubble technique. Ophthalmic Surg Lasers Imaging. 2010;41(6):642-650.
- Foroutan AR, Dastjerdi MH. Shifting-bubble sign in big-bubble technique in deep anterior lamellar keratoplasty. Cornea. 2007;26(1):117.
- Parthasarathy A, Por YM, Tan DT. Using a “small bubble technique” to aid in success in Anwar’s “big bubble technique” of deep lamellar keratoplasty with complete baring of Descemet’s membrane. Br J Ophthalmol. 2008;92(3):422.
- Sharma N, Kumar C, Mannan R, Titiyal JS, Vajpayee RB. Surgical technique of deep anterior lamellar keratoplasty in descemetoceles. Cornea. 2010;29(12):1448-1451.
- Sharma N, Jhanji V, Titiyal JS, Amiel H, Vajpayee RB. Use of trypan blue dye during conversion of deep anterior lamellar keratoplasty to penetrating keratoplasty. J Cataract Refract Surg. 2008;34(8):1242-1245.
- Luengo-Gimeno F, Tan DT, Mehta JS, Evolution of deep anterior lamellar keratoplasty (DALK), Ocul Surf. 2011;(2);98-110.
- Mannan R, Jhanji V, Sharma N, Pruthi A, Vajpayee RB. Spontaneous wound dehiscence after early suture removal after deep anterior lamellar keratoplasty. Eye Contact Lens. 2011;37(2):109-111.
- Abou-Jaoude ES, Brooks M, Katz DG, Van Meter WS. Spontaneous wound dehiscence after removal of single continuous penetrating keratoplasty suture. Ophthalmology. 2002;109(7):1291-1296.
- Abdelkader A, Kaufman HE. Descemetic versus pre-descemetic lamellar keratoplasty: clinical and confocal study. Cornea. 2011;30(11):1244-1252.
- Lee WB, Mannis MJ. The return of lamellar keratoplasty. Vis Panamerica. 2009;8:164-167.









