Corneal topographic screening of patients prior to refractive surgery ensures patients who have pre-existing corneal abnormalities, such as contact lens warpage, are properly managed, and patients who are not good candidates, due to corneal disorders, are counseled appropriately about why they should not have surgery.1 Other diseases contraindicated in laser vision correction that should be detected with corneal topography include pellucid marginal degeneration (Figure 1) and Terrien’s marginal degeneration (Figure 2). Any laser vision correction procedure, even PRK, in these latter conditions usually results in rapid biomechanical weakening of the cornea, and progression of irregular astigmatism.

Here, we provide tips on how to acquire accurate data from corneal topography. A caveat: None of the diagnostic approaches presented here or elsewhere guarantee 100% freedom from adverse events following refractive surgery. However, a combination of corneal topography, patient specific data (age, refractive error, and corneal pachymetry),2 AI-based algorithms, and corneal biomechanics-based calculations, such as the percent tissue altered (PTA) calculation, can help guide the surgeon’s choice of management.
1. Use a Fixed Scale
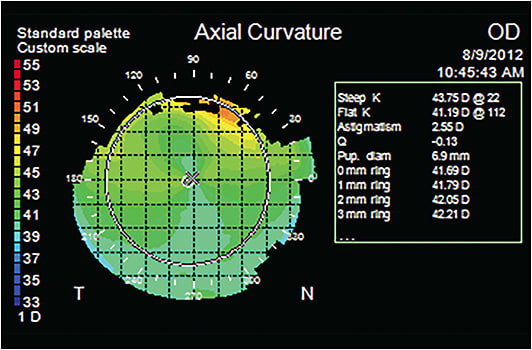
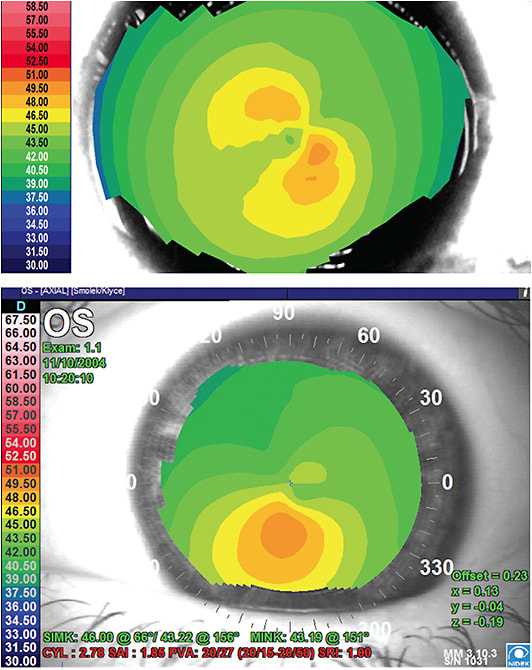
We recommend using a 1.0 D or 1.5 D fixed scale, with green scale colors being over the 43 D to 45 D of corneal curvature, i.e., centered on the average curvature for normal subjects.(Figure 3)3 Using standardized scales to facilitate interpretation also applies to wavefront analysis of the eye.4
Our reasoning for the fixed scale: If a 0.5 D or variable scales are used, normal corneas can appear to have irregular astigmatism.4,5 Also, a lot of important pattern recognition information, such as that gained from color-coded contour maps is lost when a variable scale is used. This pattern recognition facilitates the identification of steep or flat corneas, clinically significant irregular astigmatism, forme fruste keratoconus, and clinical keratoconus, among other corneal topographic abnormalities.
A caveat: If irregular astigmatism persists with the use of fixed scales that have 1.0 D or 1.5 D intervals, this could also be a reflection of imperfections in the tear film, often due to dry eye disease (DED). Software options are available on some corneal topographers to assess tear film quality, and non-invasive tear break-up time.6
When un-preserved tears are used to improve a topography examination, this should be noted in the chart, as some formulations alter curvature measurements.7 It is important that DED is managed prior to laser vision correction, as laser vision correction can confound wavefront-driven ablations, exacerbate DED, complicate visual recovery, and decrease patient satisfaction with the visual outcome. (See https://bit.ly/3yERo65 .)
2. Employ a Contrasting Color Pallete
Without distinct color contrast separating curvature intervals, significant irregular astigmatism and diagnostic cues are muted.8 We have found that the use of warm colors (yellow, orange, red) to indicate corneal areas of higher dioptric powers, and cooler colors (blue, cerulean) to represent corneal areas of lower dioptric powers provides us with essential, instinctive clues for the interpretation of corneal topography.
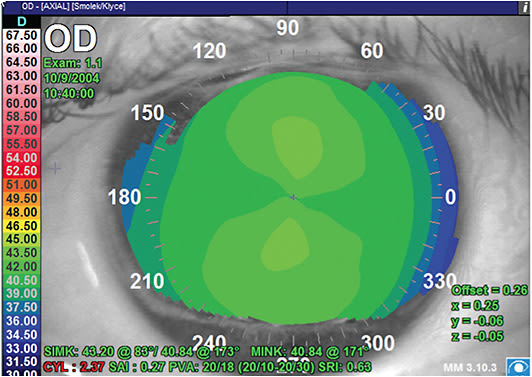
3. Prescribe Ceasing Contact Lens Wear
We have discovered that most patients who present for laser vision correction screenings wear contact lenses. As contact lens wear can cause corneal warpage (i.e., subtle, or not-so-subtle, signs of corneal irregularity or asymmetry, including inferior steepening) (Figure 4) that alters the refraction, we suggest soft contact lens wearers cease wear at least 3 days prior to corneal topography. Additionally, we recommend patients wearing gas permeable or polymethyl methacrylate lenses stop wear 1 month before their refractive surgery screening.9,10
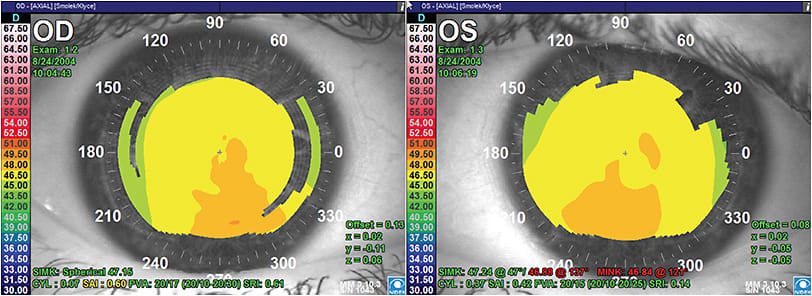
Warpage-related topographic abnormalities are likely to affect the outcomes of the surgery, since unpredictable changes in corneal contour will continue after surgery and, at the least, will increase the need for re-treatment, if not the incidence of permanent irregular astigmatism and associated loss of best spectacle-corrected visual acuity.
If signs of corneal warpage are detected at the refractive surgery screening, we suggest discontinuing contact lens wear, and monitoring the corneas for resolution of warpage before proceeding with refractions and wavefront analyses that will be used in the excimer laser ablation.
In most eyes, the warpage will resolve. The amount of time that takes varies immensely, especially in hard or gas permeable contact lens wearers. If the irregularity never resolves after contact lens-wear discontinuation, then refractive surgery is usually not a good option for that eye. Taking the time to properly manage these contact lens-wearing candidates improves refractive surgery outcomes.
4. Utilize Indices
To identify keratoconus suspects, clinical keratoconus, keratoglobus, pellucid marginal degeneration, and Terrien’s marginal degeneration, among other disorders that produce topographic abnormalities that portend a poor outcome for refractive surgery, we recommend utilizing indices, such as the keratoconus prediction index,11 the keratoconus severity index,12 AI-based classifications,13,14 and/or the inferior-superior (I-S) index. Some corneal topography instruments automatically provide these indexes. As we, the authors, often use the I-S Index, we will briefly describe it.
The I-S Index (Figure 5) is the dioptric power difference of the average of 5 points of the inferior map (vertical 0° axis at 3 mm and points 30° and 60° on both sides of the 0° axis, that are also at 3 mm), and the dioptric average of five mirroring points of the superior map.15
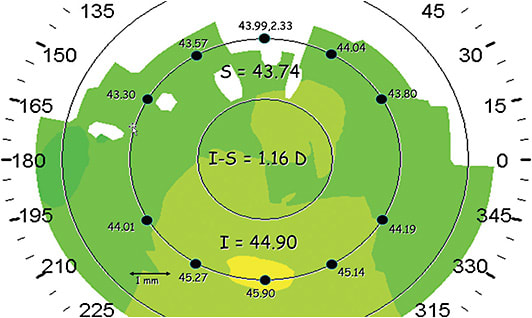
Corneas that have an I-S Index less than or equal to 1.4 D are more likely to have normal inferior steepening, especially if that is the case in both eyes.
In one of the author’s experience, performing PRK in eyes that have inferior steepening where the I-S index is less than or equal to 1.4 D is usually safe, as the incidence of cornea ectasia is low, and the outcomes are typically excellent in such eyes.16,17
Eyes with an I-S index greater than 1.4 D, or that are diagnosed with an ectatic pathology (Figure 6A, B) should not be considered candidates for PRK, LASIK, LASEK, or SMILE,18,19 except possibly in an Institutional Review Board-approved clinical trial of laser vision correction in keratoconus, accompanied by riboflavin-UV cross-linking.
5. Consider Using the PTA Calculation
Another useful tool to analyze data from corneal topography is the PTA calculation.20,21 PTA = (flap thickness + ablation depth)/central corneal thickness. For LASIK candidates, the maximal flap thickness + ablation depth should not exceed 40% (PTA < 0.40). If the PTA could exceed 0.40, PRK may be a better choice for otherwise normal corneas.
However, many surgeons recommend that final central corneal thickness not end up less than 400 µm even after PRK surgery.
Due Dilligence Required
As illustrated in this article, corneal topographic analysis is a critical part of the surgeon’s preoperative screening exam to aid in the detection and management of pre-existing corneal abnormalities. Doing so enables patients who have contraindications to be excluded from refractive surgeries that would result in poor outcomes. CP
References:
- Wilson SE, Klyce SD. Screening for corneal topographic abnormalities before refractive surgery. Ophthalmology. 1994;101:147-152.
- Randleman JB, Banning CS, Stulting RD. Corneal ectasia after hyperopic LASIK. J Refract Surg. 2007;23(1):98-102.
- Smolek MK, Klyce SD, Hovis JK. The Universal Standard Scale: proposed improvements to the American National Standards Institute (ANSI) scale for corneal topography. Ophthalmology. 2002;109(2):361-369.
- Smolek MK, Klyce SD. Absolute color scale for improved diagnostics with wavefront error mapping. Ophthalmology. 2007;114(11):2022-2030.
- Wilson SE, Klyce SD, Husseini ZM. Standardized color-coded maps for corneal topography. Ophthalmology. 1993;100(11):1723-1727.
- Goto T, Zheng X, KLyce SD, et al. Evaluation of the tear film stability after laser in situ keratomileusis using the tear film stability analysis system. Am J Ophthalmol. 2004;137:116-120.
- Novak KD, Kohnen T, Chang-Godinich A, et al. Changes in computerized videokeratography induced by artificial tears. J Cataract Refract Surg. 1997;23:1023-1028.
- Maguire LJ, Singer DE, Klyce SD. Graphic presentation of computer analyzed keratoscope photographs. Arch Ophthalmol. 1987;105(2):223-230.
- Wilson SE, Lin DT, Klyce SD, Reidy JJ, Insler MS. Topographic changes in contact lens-induced corneal warpage. Ophthalmology. 1990;97(6):734-744.
- Ruiz-Montenegro J, Mafra CH, Wilson SE, Jumper JM, Klyce SD, Mendelson EN. Corneal topographic alterations in normal contact lens wearers. Ophthalmology. 1993;100(1):128-134.
- Maeda N, Klyce SD, Smolek MK, Thompson HW. Automated keratoconus screening with corneal topography analysis. Invest Ophthalmol Vis Sci. 1994;35(6):2749-2757.
- Smolek MK, Klyce SD. Current keratoconus detection methods compared with a neural network approach. Invest Ophthalmol Vis Sci. 1997;38(11):2290-2299.
- Maeda N, Klyce SD, Smolek MK. Neural network classification of corneal topography: preliminary demonstration. Invest Ophthalmol Vis Sci. 1995;36(7):1327-1335.
- Klyce SD, Karon MD, Smolek MK. Screening patients with the corneal navigator. J Refractive Surg. 2005;21:S617-S622.
- Rabinowitz YS, McDonnell PJ. Computer-assisted corneal topography in keratoconus. Refract Corneal Surg. 1989;5(6):400-408.
- Bilgihan K, Ozdek SC, Konuk O, Akata F, Hasanreisoglu B. Results of photorefractive keratectomy in keratoconus suspects at 4 years. J Refract Surg. 2000;16(4):438-443.
- Sun R, Gimbel HV, Kaye GB. Photorefractive keratectomy in keratoconus suspects. J Cataract Refract Surg. 1999;25(11):1461-1466.
- Mattila JS, Holopainen JM. Bilateral ectasia after femtosecond laser-assisted small incision lenticule extraction (SMILE). J Refract Surg. 2016;32(7):497-500.
- Binder PS. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29(12):2419-2529.
- Santhiago MR, Smadja D, Gomes BF, et al. Association between the percent tissue altered and post-laser in situ keratomileusis ectasia in eyes with normal preoperative topography. Am J Ophthalmol. 2014;158(1):87-95.
- Santhiago MR, Wilson SE, Smadja D, Chamon W, Krueger RE, Randleman JB. Validation of the percent tissue altered as a risk factor for ectasia after LASIK. Ophthalmology. 2019;126(6):908-909.










