For cataract surgery patients who underwent RK and LASIK, and desire blended vision, or patients who have irregular corneas, which make obtaining accurate biometry readings difficult, IOL selection has been a challenge. The Light Adjustable Lens (LAL) (RxSight) can overcome this challenge. Specifically, this IOL can be tailored to the patient’s visual needs via the company’s Light Delivery Device (LDD) postoperatively, allowing for satisfactory outcomes. (See www.rxsight.com/us ).
Here, I discuss how to implement this IOL in one’s practice successfully:
Know the Clinical Pearls
Before offering this IOL, we should be aware of the following clinical pearls:
- Systemic medication use can be a contraindication. The LAL is contraindicated in patients who are using a systemic medication that may increase sensitivity to UV light or that is considered toxic to the retina (e.g., tamoxifen). Thus, it is important to contact the patient’s prescribing doctor to see whether the patient can stop such medications 1 to 2 weeks prior to this cataract procedure.
- Shoot for a dilation of 6 mm. This is so we are able to actually see the optic-haptic junction, and treat the entirety of the lens when making the light adjustments.
- Compliance with UV-protective glasses is a must. LAL patients must be able to adhere to wearing UV-protective glasses until their final LDD treatment. Typically, the median time for full treatment is 4 weeks. Pro tip: Have the patient bring a family member with them to their first postop visit to reinforce the importance of wearing these glasses. At this visit, reemphasize that if the LAL gets exposed to UV light, it can cause uncontrolled changes to the IOL that may result in the need to replace it. (Incidentally, RxSight is launching a new lens that has built-in UV protection intended to reduce this compliance burden during the postoperative adjustment period, according to the company.)

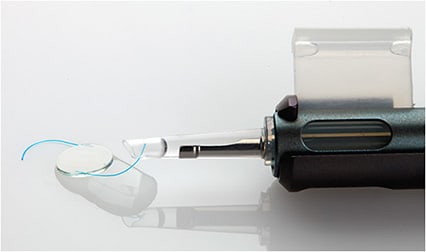
The Light Adjustable LensIMAGE COURTESY RXSIGHT - Hold off on early YAG treatment. I would not recommend performing YAG laser treatment early to get the LAL into the final lens position. This is because the patient may not be completely happy with the visual result. I’ve had a few post-RK patients who I, perhaps, locked in a little too early, and they had a bit of a shift, and may need occasional contact lenses or glasses, such as for driving, with a very small prescription, usually less than 1 D.
- Extend the adjustment timing for RK patients. The longer these patients are out from their cataract surgery, the better. As a result, I recommend extending the timing of the first LDD to at least 4 or 5 weeks postop (versus 3 weeks for virgin or post-LASIK corneas), and to wait at least 1 week in between adjustments (versus 3 days).
Provide Patient Education
There is a learning curve with the patient consultation: how you refine the words and phrases used to describe the LAL, making sure to be very clear about why you’re prescribing it and how it’s different, and setting the appropriate expectations.
- Describing the LAL. When I think the LAL is the best option for a patient, I don’t discuss all the other IOL options because doing so can be unnecessarily confusing for the patient. I say, “Because your eyes are somewhat abnormal and you’ve had other surgical procedures, our best chance of getting you the best possible vision is with what’s called the Light Adjustable Lens. This has been a revolution in cataract surgery because its prescription can be adjusted after it’s been implanted in the eye. In the past we’ve had to use surgical techniques, such as a LASIK touch-up or lens exchange, to home in on the refractive target. With LAL, no touch-up surgery is needed. This is what I would do for my own eye.”Next, I discuss the fact that the LAL more than doubled the chance of achieving 20/20 vision at distance. (See www.rxsight.com/us .) After that, I discuss the postoperative visits required to perform the LDD, and the need to wear UV-protective glasses until the final adjustment. There will be questions about the financial aspect, and for some patients the cost of the LAL can be out of their reach.
- Determine the refractive correction. The patient needs to decide whether they want blended vision or be matched up for distance. Patients who have been in blended vision for years tend to keep it. If they haven’t been, we tend to focus on distance.
- Set appropriate expectations. This is a balancing act. On the one hand, we want to be enthusiastic in recommending the LAL. On the other hand, we don’t want to oversell it too much, as certain patients may not achieve the vision they think they will. For example, some patients — even some with only a 4- or 8-cut RK — who have a lot of corneal aberrations, scarring, and irregularities, could still have visual fluctuation even with the LAL. Additionally, patients who have 8- or 16-cut RK are going to have a long postoperative course, and may have some visual fluctuations. The bottom line is that patients need to be made aware that while their friends or family members who have the LAL may have achieved “perfect vision,” their case could be different. The LAL is not perfect in certain corneas. Something else to educate patients on: Post-LAL eyes can dilate slower than they did prior, so LDD treatment visits can take longer than expected.

Determine Workflow Integration
When it comes to the postoperative end of LAL, it makes sense to determine when LDD treatments can be fit into the schedule — before, during, or after clinic — and who’s going to do these treatments.
I find that workflow integration tends to work best if the ophthalmologist has support in performing LDD. In my practice, for example, the ophthalmic physician’s assistant (PA) does the majority of the light adjustments. Initially, I performed the adjustments myself, and would schedule the patients during clinic hours, but I discovered seeing patients and LDD patients was too difficult. Having my PA perform some of the light adjustments helps the workflow run smoother. If you have support staff, such as an optometrist or a PA, perform the adjustments, remember to explain that to patients up-front, so that they’re not surprised and, therefore, dissatisfied that their surgeon isn’t doing the adjustments.
LAL Experience
My patients have been very pleased with the quality of their distance vision, and a lot of them have remarked that their vision is similar to what it was after they underwent LASIK. That’s not something that is heard very often. With post-LASIK cataract patients, we typically have to counsel them that their IOL vision won’t be like it was with LASIK. Such patients won’t wake up the next day and see perfectly, but with the LAL, they can achieve LASIK-like outcomes. CP









