Corneal Physician Symposium Returns With Compelling Sessions
On December 11, more than 20 front-of-the-eye aficionados will be providing their anterior segment expertise at 8 online sessions during the second annual Corneal Physician Symposium, formerly known as the Cornea Virtual Summit. The content, which offers 6 CME credits, has been amassed by returning course directors, Kendall E. Donaldson, MD, MS, and Cynthia Matossian, MD.
The meeting agenda is comprised of medical and surgical cornea sessions, which can be accessed at www.cornealphysician.com/corneal-physician-symposium/agenda . For additional information, including registration, visit www.cornealphysician.com/cps , email eventhelp@pentavisionmedia.com, or phone: (215) 237-9128.
Ophthalmologist to be Inducted Posthumously Into the National Inventors Hall of Fame

Dr. Patricia Era Bath (1942 to 2019), will be celebrated at two ceremonies in 2022 for inventing the Laserphaco Probe for cataract treatment in 1986. The first is an “Illumination Ceremony” at the National Inventors Hall of Fame Museum, in Alexandria, Va., on May 4th, and the second is the 2022 National Inventors Hall of Fame (NIHF) “Induction Ceremony” in Washington, D.C. on May 5th. Dr. Bath is one of two Black women inventors to ever be inducted by the NIHF.
“To know that my mother is part of the 2022 class of National Inventors Hall of Fame inductees is an unbelievable honor,” says Dr. Eraka Bath, a psychiatrist, to the NIHF. “Her incredible career path – and her contributions to the study of ophthalmology, cannot be understated. The NIHF distinction is an overdue recognition of her accomplishments.”
In addition to inventing a device that streamlined cataract surgery, Dr. Bath became the first known Black women to receive a medical patent [U.S. Patent No. 4,744,360] — 1 of 8 in her career — was the first Black person to complete an ophthalmology residency at New York University in 1973, and the first Black American woman named to the UCLA Medical Center surgical staff in 1974. Additionally, she established the American Institute for the Prevention of Blindness with the goal of eradicating preventable blindness in minority populations. For additional information on Dr. Bath, visit https://drpatriciabath.com .
Cataract, Among Other Eye Conditions, Linked with Increased Risk of Dementia
Patients who have AMD, cataract, or diabetes-related eye disease (DRED) are at a greater risk of dementia, and individuals who have both ophthalmic and systemic conditions are at a higher risk of dementia vs. those with an ophthalmic or systemic condition alone, reported the British Journal of Ophthalmology.1
Specifically, of more than 1,263,513 person-years of follow up, 2,304 cases of incident dementia were recorded. In breaking it down by eye condition, the multivariable-adjusted HRs (95% CI) for dementia linked with AMD, cataract and DRED, and glaucoma at baseline were 1.26 (1.05 to 1.52), 1.11 (1.00 to 1.24), 1.61 (1.30 to 2.00), and (1.07 (0.92 to 1.25), respectively. Additionally, those who had a cataract and a systemic condition were 1.19 to 2.29 times more likely to develop dementia vs. those who did not have cataract and systemic conditions. Further, diabetes, hypertension, heart disease, depression, and stroke — discovered during follow-up — mediated the link between cataract and incident dementia, as well as the link between DRED and incident dementia.
The study was comprised of 12,364 adults ages 55 to 73 from the UK Biobank cohort, who were evaluated between 2006 and 2010 at baseline, and were followed up until the beginning of 2021. Incident dementia was determined employing hospital inpatient, death records and self-reported data.
Reference
- Br J Ophthalmol. doi: 10.1136/bjophthalmol-2021-319508.
GENETIC TEST PROTOCOL: AVAGEN IN ACTION
By Mitchell A. Jackson, MD

AvaGen (Avellino Lab USA, Inc.) tests suspect patients and detects corneal conditions earlier, specifically for keratoconus (KC) and presence of corneal dystrophies (CD), allowing the patient to begin sight-saving treatment earlier. Good candidates for AvaGen include those who have a known family history of KC or CD, as well as patients who have progressive astigmatism, or are seeking refractive surgery. (As doctors know, by the time we see the physical symptoms of KC, vision has already been compromised, so early detection will help preserve sight.)
Here, I briefly discuss the test protocol:
• Acquiring the genetic sample. The doctor or qualified technician takes the swab and rolls it a sufficient number of times, and with good pressure along the inside of the cheek. Assuming this is done, the test sample should contain enough genetic material to run a quality test, and the sample is sent to Avellino’s high-complexity CLIA-certified lab for analysis. Some caveats: It is very important that the patient is notified prior to testing that they consume no milk products or coffee before collection, as this compromises the sample. Also, patients should brush or rinse out their mouth thoroughly, then wait 30 minutes without eating or drinking before their sample is collected.
• Acquiring test results. The doctor receives results in approximately 10 days via an actionable report that is sent through a HIPAA-secured patient portal. For KC, Avellino has a proprietary algorithm that determines the risk score. The testing process takes into account important factors, such as the number of positive variants and ethnicity, which helps determine the test result (a polygenic risk score) that falls in low, moderate, or high risk of KC. For corneal dystrophies, the test is a “yes” or “no” result, so one detected variant of the gene will report a definitive result for these conditions.
As a best practice, I schedule a follow-up visit with the patient, so we can review the results and, if appropriate, discuss management and intervention pathways. In addition, Avellino provides genetic counseling at no cost to both doctors and patients to provide educational information about what their genetic test result means for the patient.
Eye care practitioners can now bring precision diagnostics into their practice and, along with advanced corneal imaging, can help protect and preserve sight with early detection of KC. With a proper diagnosis, we can now have greater confidence on the most effective treatment path for patients and, in the case of refractive surgery, rule patients in or out for these surgeries.
For more on AvaGen, see this month’s “Product Spotlight,” on p.16. CP
Dr. Jackson has participated in an Avellino advisory board.
Studies Shed Light on Part of Eye That Controls Amount of Light That Enters Eye
Two studies that focus on the pupil show it’s possible to change pupil size on command, and that the eyes of computer-generated faces designed to fool the beholder contain irregular pupils, respectively.
In the first study, published in the International Journal of Psychophysiology, a 23-year-old man was able to voluntarily change his pupil size, regardless of possible indirect mechanisms of action, such as brightness, dilating to a diameter of 0.8 mm, and constricting it at about 2.4 mm. The latter didn’t change his vergence and improved his visual acuity by 6.00 D.
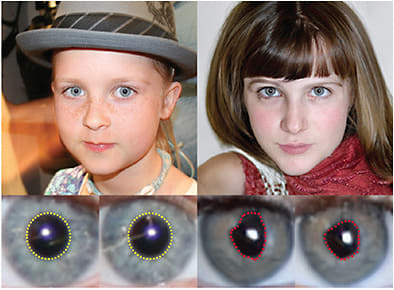
After utilizing MRI, the study’s researchers say the pupil size changes were linked with “increased activation of parts of the left dorsolateral prefrontal cortex, adjacent premotor areas, and supplementary motor area.”
In the second study, out of two state universities of New York (Albany and Buffalo), the researchers showed computer-generated faces, often referred to as “deep fakes,” which can be difficult to tell apart from real faces, can be revealed by irregular pupils.
The researchers credit the lack of physiological constraints in the “deep fake” models, and show qualitative and quantitative assessment of their method to extract the pupils, and evaluate their shapes is simple and effective. For additional information, visit https://bit.ly/3kjDSRD and https://arxiv.org/pdf/2109.00162.pdf .

Corneal Endothelium Encouraging Quantitative Index for Graves’
Active Graves’ ophthalmopathy (GO) showed morphological alterations in corneal endothelium vs. inactive GO, revealing that the cell area reflected in corneal endothelial function has the probability of acting as a non-invasive, objective, and quantitative index for assessing GO activity status, reported the American Journal of Ophthalmology.1
Specifically, the coefficient variation of cell area in corneal endothelial function was significantly higher in active GO versus inactive GO (37.0[34.4-41.2]% vs. 33.9[30.9-36.8]%, P=0.001), and positively correlated with clinical activity score (CAS) (r=0.322, P<0.001). Also, cell area had the capacity to differentiate active GO eyes from inactive GO eyes.
This study was comprised of 128 eyes of 64 GO patients. Each eye was given a specific CAS, and then labeled as Active (CAS ≥ 3 points) or Inactive (CAS < 3 points). The researchers used generalized estimating equations, that accounted for inter-eye correlation, to compare the ocular parameters between the two groups. Receiver operating characteristic curves were also obtained.
Reference:
- Am J Ophthalmol. doi: 10.1016/j.ajo.2021.05.020.
STOCK.ADOBE.COM / EUNIKAS
Using Solid Fuel Long-Term to Cook Raises Risk of Anterior Eye Conditions
Cooking with solid fuel (e.g., coal or wood) long-term is linked with higher risks of conjunctiva disorders, cataracts, sclera, cornea, iris, and ciliary body disorders (DSCICs), and cases of glaucoma, reported PLOS Medicine.1
Specifically, compared with those who used clean fuel (e.g., electricity or gas), solid fuel users had adjusted odds ratios (ORs) of 1.32 (1.07 to 1.37, p < 0.001) for conjunctiva disorders, 1.17 (1.08 to 1.26, p < 0.001) for cataracts, 1.35 (1.10 to 1.66, p = 0.0046) for DSCICs, and 0.95 (0.76 to 1.18, p = 0.62) for glaucoma.
Additionally, switching from solid to clean fuels was linked with less increased risks (over long-term clean fuel users), with adjusted ORs of 1.21 (1.07 to 1.37, p < 0.001), 1.05 (0.98 to 1.12, p = 0.17), and 1.21 (0.97 to 1.50, p = 0.088) for conjunctiva disorders, cataracts, and DSCICs, respectively.
What’s more, the adjusted ORs for the eye conditions were “broadly similar” in those who used solid fuel, despite ventilation status.
The researchers arrived at these findings after drafting 512,715 adults, ages 30 to 79, from 10 areas in China during 2004 to 2008, and asking them via questionnaire their cooking frequency and primary fuel types for doing so. Amid median (10.1 [9.2 to 11.1]) years of follow-up, electronic linkages to national health insurance databases revealed 4,877 cases of conjunctiva disorders, 13,408 cataracts, 1,583 of DSCICs, and 1,534 incidences of glaucoma. The researchers adjusted for confounding factors, such as age at baseline, alcohol use, birth cohort, body mass index, cookstove ventilation, education, environmental tobacco smoke, heating fuel exposure, length of recall period, occupation, prevalent diabetes, self-reported general health, sex, smoking, and study area.
As there is narrow evidence from cohort studies on the links between using solid fuels and major eye diseases, the researchers sought to perform this study. They note that over 3.5 billion individuals worldwide are exposed to household air pollution that comes from solid fuel use.
The study’s researchers say the main limitations of this study were a lack of baseline eye disease assessment, the use of self-reported cooking frequency and fuel types, the risk of bias due to delayed diagnosis (especially for cataracts), and potential residual confounding from unmeasured factors (e.g., sunlight exposure).
Reference:
- PLOS Medicine. https://doi.org/10.1371/journal.pmed.1003716 .
Immediate Sequential Bilateral Cataract Surgery Linked With Worse Visual Outcomes
Immediate sequential bilateral cataract surgery (ISBCS) is associated with worse visual outcomes, which may or may not be clinically meaningful, depending on a patient’s additional risk factors, reported a recent retrospective cohort study in JAMA Ophthalmol.
Specifically, in accounting for age, self-reported race, insurance status, history of AMD, diabetic retinopathy, and glaucoma, the uncorrected visual acuity (UCVA) was lower by 2.79 (95% CI, -2.95 to -2.63; P < .001) letters, and the best-corrected visual acuity (BCVA) by 1.64 (95% CI, -1.74 to -1.53; P < .001) letters in the ISBCS group, whereas the UCVA of the first surgical eye was higher by 0.41 (95% CI, 0.36-0.45; P < .001) letters, and the BCVA was higher by 0.89 (95% CI, 0.86-0.92; P < .001) letters in the delayed sequential bilateral cataract surgery (DSBCS) group. Additionally, in the second eye, the UCVA was lower by -1.67 (95% CI, -1.83 to -1.51; P < .001) letters, and the BCVA by -1.88 (95% CI, -1.98 to -1.78; P < .001) letters in the ISBCS group versus the DSBCS group, where the UCVA was higher by 0.79 (95% CI, 0.74-0.83; P < .001) letters, and the BCVA by 0.48 (95% CI, 0.45-0.51; P < .001) letters. The study was comprised of data from 1,824,196 patients (mean [SD] age for those < 87 years, 70.03 [7.77]; 684 916 [37.5%] male) with bilateral visual acuity measurements who underwent bilateral cataract surgery, and were on the American Academy of Ophthalmology Intelligent Research in Sight (IRIS) Registry.
The study’s researchers note “nonrandom surgery group assignment, confounding factors, and large sample size could account for the small but statistically significant differences noted,” so additional studies are needed to determine whether these factors should be considered clinically relevant when counseling patients before cataract surgery.
Reference:
- JAMA Ophthalmol. doi:10.1001/jamaophthalmol.2021.2032.
Chronic Graft-Versus-Host Disease Patients Using Glaucoma Drops At Greater Risk of Corneal Perforation
Patients who have chronic graft-versus-host disease (GVHD) who use topical antiglaucoma drugs should be monitored closely for corneal perforation, as they are at higher risk for the rare, vision-threatening complication linked with chronic GVHD, reported Cornea.1
Specifically, the researchers assessed the case records of 405 chronic GVHD patients over 8 years, and reviewed the preponderance of corneal perforation in the group. Additionally, the researchers looked at patient demographics, indication for and type of hematopoietic stem cell transplantation (HSCT), time elapsed between HSCT and perforation, and clinical features, such as GVHD severity scores, ocular comorbidities, and topical medication use at the time of perforation. CP
Reference:
- Cornea. DOI: 10.1097/ICO.0000000000002526
Also Noteworthy
- Aurion Biotech, a company whose mission is to cure blindness by developing a differentiated platform of advanced therapies to treat ocular diseases, announced positive preliminary findings from its proof-of-concept IOTA trial, comprised of 50 corneal endothelial disease patients who were treated with a cell therapy procedure. Specifically, patients have shown improvements in visual acuity and central corneal thickness, and this procedure is accessible for surgeons, and minimally invasive for patients. In other news, the company appointed Shigeru Kinoshita, MD, PhD, inventor of the cell therapy procedure for corneal endothelial disease, a member of its medical advisory board; Greg Kunst, CEO; and Edward Holland, MD, was named chief medical advisor.
- BVI is entering a collaborator relationship with Beyeonics Vision that would support Beyeonics Vision’s efforts to streamline the U.S. commercialization of an upgradable digital visualization system that replaces traditional microscopes. Called Beyeonics One, the system is equipped with an ultra-high-resolution camera in which processed and digitally enhanced images are transferred to high-resolution, head-wearable displays, for an immersive and natural stereoscopic 3D-viewing experience for surgeons. Additionally, Beyeonics One allows for customizable integration of accessible pre/intra-operative data, and integration with other devices, the company says.
- EyeGate Pharmaceuticals, a clinical-stage company creating and commercializing products for treating inflammatory and immune diseases, with a focus on the eye and nervous system, named Brian M. Strem, PhD, co-founder, director, and former CEO of Okogen, Inc. as well as co-founder and managing director of Bayon Therapeutics, permanent president, chief executive officer, and board member, effective immediately. Dr. Strem has strategic expertise, scientific acumen, and drug development experience in ophthalmology, otology, and regenerative medicine, the company says. In other news, EyeGate entered a non-binding letter of intent to purchase Bayon Therapeutics, which is a private ophthalmic specialty pharmaceutical company focused on utilizing light-sensitive “photoswitch” small molecules created to restore vision in patients who have inherited and age-related degenerative retinal diseases.
- Euclid Systems, a company that makes products for myopia management, named Vance Thompson, MD, chief medical officer. Dr. Thompson is a recognized authority in laser vision correction and advanced cataract surgery, and has served as the medical monitor lead or principal investigator in several FDA-monitored clinical trials, the company says. He is the founder of Vance Thompson Vision, in Sioux Falls, SD, and professor of ophthalmology at the University of South Dakota’s Sanford School of Medicine.
- Harrow Health Inc. entered into an agreement with Sintetica, S.A., a pharmaceutical company focused on analgesics, local anesthetics, and sterile injectable solutions, to acquire the marketing and supply rights in the United States and Canada for AMP 100, an ocular surface anesthetic drug candidate for surgeries, such as cataract surgery, and intravitreal injections. Sintetica intends to submit a New Drug Application to the FDA in late 2021.
- Hilco Vision (www.hilcovision.com ), a global vision care company that provides various ophthalmic products, such as optical tools, purchased Bruder Healthcare LLC. Bruder (www.bruder.com ) delivers therapeutic and ophthalmic products, such as eye compresses and lid hygiene cleansers, to medical professionals and consumers, broadly available under the Bruder and Thermalon brands. The business will continue to be based out of Alpharetta, Ga.
- Johnson & Johnson Vision announced the global availability of its VERITAS Vision System, a phacoemulsification device created to address patient safety, surgeon efficiency, and comfort. The System features include less surge, more stability; Hybrid Fluidics Technology (to minimize post-occlusion surge to protect intraocular structures and provide chamber stability); Intelligent Occlusion Sensing Technologies that automatically respond to occlusions to preserve a calm, stable chamber, even in dense cataract cases; and an ergonomically designed foot pedal for total control and a more comfortable experience, the company says. In other news, Johnson & Johnson Vision announced the availability of TECNIS Synergy and TECNIS Synergy Toric II IOLs in the United States and Canada. The IOLs deliver a wide range of continuous vision, near vision, image contrast, high satisfaction with nighttime activities, and a reduced need for glasses, Johnson & Johnson Vision says. For more information, visit www.beyondcataracts.com .
- Luneau Technology Group announced it has merged with Optovue Inc. Founded by Jay Wei in 2003, Optovue develops high-speed OCT and OCT-A technology to aid in diagnosing and managing eye diseases. Luneau Technology came out with wavefront-based diagnostic and finishing solutions, and developed automated solutions for the past 15 years. Dr. Marc Abitbol, CEO of Luneau Technology, will preside over the newly merged company, while Optovue CEO Peter Wyles will join the global leadership team.
- Merakris Therapeutics reached an agreement with Miracles In Sight (MIS), a large non-profit eye bank, to supply Opticyte Amniotic Ophthalmic Repair Grafts to MIS-affiliated eye surgeons in North and South Carolina, and Texas. Opticyte Grafts provide a biological barrier to protect the corneal surface during healing, and aid in preventing the formation of scar tissue, the company says. Additionally, the Graft supports cell attachment and ingrowth, and is commonly used as a supplemental biological barrier in dry eye disease, or other corneal defects. The Grafts, derived from amniotic membrane, are available in different shapes and sizes to address a variety of surgical needs. For more information, visit www.merakris.com .
- NovaBay Pharmaceuticals, Inc. entered into a definitive agreement to acquire DERMAdoctor, LLC, a privately held company that commercializes dermatologist-developed skincare products, including all of its inventory, products, and intellectual property, for $15.0 million, comprised of $12.0 million in cash at closing and up to an additional $3 million in earnout payments contingent upon the DERMAdoctor business achieving predetermined financial targets for the 2022 and the 2023 fiscal years. NovaBay says it plans for the DERMAdoctor business to continue its operations from its current headquarters in Riverside, Mo. The companies say they are targeting a closing of the transaction in the fourth quarter 2021.
- Ocuphire Pharma, Inc. appointed Jay S. Pepose, MD, PhD, to its board of directors as a director. Dr. Pepose, founder and current medical director of the Pepose Vision Institute, a 2-location practice in Missouri, and professor of clinical ophthalmology and visual sciences at Washington University School of Medicine, in St. Louis, was already a member of the company’s medical advisory board, where he has contributed to clinical programs by providing advice on drug development and regulatory strategy, and mid-to- late-stage clinical trial design, Ocuphire Pharma, Inc. says.
- RxSight, Inc. named three new members to its board of directors. They are Robert (Bob) Palmisano, Robert Warner, and Julie Andrews. Mr. Palmisano was president and CEO of Wright Medical Group, Inc. from 2011 to 2020. Mr. Warner served as a member of the Alcon Executive Leadership Team for over 10 years. Ms. Andrews was a senior vice president, Global Finance, and chief accounting officer at Wright Medical Group, Inc. from 2012 to 2020. In other news, the company appointed Steve Everly as its vice president of U.S. sales. Mr. Everly comes from Johnson & Johnson Vision, where he served as Area vice president, Surgical Sales Western U.S., and was responsible for all aspects of cataract, refractive, and ocular surface product sales.
- Tarsus Pharmaceuticals, Inc. appointed Rosemary A. Crane to its board of directors. She will be chair of the newly created Science and Technology Committee, fo-cused on external and internal innovation, and pipeline opportunities, the company says. Ms. Crane has 30 plus years of experience in the pharmaceutical industry, including in executive leadership, and global commercialization expertise, the company says. CP








