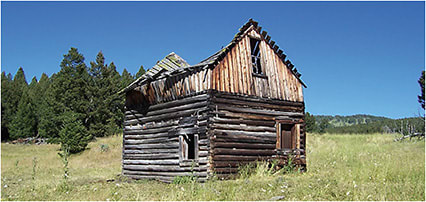
Being the granddaughter of Montana cattle ranchers has given me a heritage rich in integrity, grit, graciousness, and gumption. The land and my experiences hold a special place in my heart. It’s the place where barns are raised as a community, and you stop to help strangers. The Continental Divide headwaters, just 30 miles upstream, feed the river that runs through the land. I remember my grandpa could sense the weather changes before anyone else. He was also the farrier for the valley, and was famous for gracefully shoeing even the orneriest horse. My grandma was second-generation Norwegian, owned the town cafe, made thousands of pies in her lifetime, and put herself through college in her 40s.
I knew at age 12 I wanted to be a physician, and ophthalmology is the perfect fit in retrospect. I remember spending countless hours looking at the eyes of the horses, cattle, bees, fish, and bugs I’d encounter. I was the curious kid who constantly wanted to learn how things worked and why. I suspect that may have made me challenging to parent, but that curiosity has served me well as a molecular immunobiologist (prior to medical school), and as the founder of a private practice dedicated to the needs of and solutions for our amazing dry eye disease (DED) patients. Grandpa would say, “You can’t ride a 3-legged horse,” by which he meant, it takes four legs of a good horse for getting where you need to go. And where you decide to go is just as important. I set my sights on creating a DED clinic with the needs of the DED patient at its very center.
Here are the four legs of how I rode into the incredible landscape of the advanced DED practice during the start of the COVID-19 pandemic.
1. Star Power
I don’t mean in the Box Office sense, but in the stargazing sense. Specifically, keeping an eye on the horizon ahead and gazing above at the bright spots in the development of our scientific knowledge, and clinical tools enables us to best manage our DED patients. How can we accomplish this? The answer is consistent education via reading related journal articles, attending DED lectures and eye care-related events (ARVO, ASCRS, AAO, AECOS, WIO, WCC, etc.), networking with colleagues, and sharing our own research. (Having studied inflammation for 31 years, I hope the review papers I’ve written help colleagues to bridge the turbid waters of sign/symptom disconnect in DED.) 1,2
Expanding disease state knowledge to common neurologic, systemic and autoimmune comorbidities, such as migraine headaches, post-surgical and postrefractive DED, obstructive sleep apnea and rosacea, as well as Sjögren’s syndrome, helps create a framework for seeing the connections, leveraging the interventions, and incorporating the innovations to meet these patients’ needs. Nutrition, hydration, lifestyle, and personal habits play a surprising role in DED. Dermatology, aesthetics, and ophthalmology have multiple overlaps with respect to DED. Additionally, a deeper understanding of the immunopathophysiology of DED and meibomian gland dysfunction (MGD), and the mechanisms of action of the excellent medications available are well within reach for every ophthalmologist who wants to learn more.1,2

2. Fire Power
This is where a deep understanding of the tools and the disease state come in to play. Rapid improvements in symptoms, osmolarity, inflammation, staining, tear break-up time, and more are achieved with the “fire power” of advanced diagnostic devices and in-office treatments. Specifically, tear quality measurement devices, tear quantity measurement devices, and ocular surface structural analysis devices are available to aid in arriving at a definitive diagnosis, which, then, lends itself to prescribing the most appropriate treatment(s).
In building my DED practice, I have been sure to offer in-office advanced diagnostic testing (tear osmolarity, MMP-9, meibography, etc.), as well as advanced in-office treatments, such as intensive eyelid cleaning, intense pulsed light (IPL), and device-based meibomian gland expression.
I started offering all these services and more in a 200 square-foot room. The first IPL treatment is often performed at the end of the first 90-minute comprehensive appointment, and specifically, we use the OptiLight IPL (Lumenis), which has FDA approval for improving and managing DED associated with MGD. Most patients receive four in-office OptiLight treatments spaced 2 to 4 weeks apart to achieve excellent improvements in their ocular surface signs and symptoms. Very severe cases receive more sessions and achieve improvements, particularly as part of a comprehensive, integrated treatment plan following the Tear Film & Ocular Surface Society Dry Eye Workshop II and ASCRS guidelines.
Of course, having good equipment at home also helps patients on their journey. The availability of carefully curated items in the clinic helps patients succeed with their home care.
3. Creative Power
In setting up the practice, my staff and I cobbled together different, affordable information technology innovations in patient intake forms, scheduling, telemedicine, EMR, and practice management. Each IT solution was chosen with patient satisfaction, and efficiency at the forefront. We chose an internal medicine EMR for its affordability, customizability, patient communications portal, and completeness. Additionally, we selected a HIPAA-compliant, cloud-based system with a great user interface that enables patients to easily complete their intake forms (lengthy due to the complexity of DED contributors), submit telemedicine photos, and sign office policy acknowledgments, consent forms for procedures, and clinical research studies with a simple link, website click box or QR code. Further, the cloud-based system can take any PDF and turn it into a mobile form with a great user interface that works from any computer, or smart phone.
4. Heart Power
Heart power is the source of compassion, but also the source of endurance and perseverance on even the longest days, and the toughest cases. Heart power is also listening and leaning in to each patient’s journey, and this compass is full of rewards for patients, doctors, and staff. Creating time and space for communications with and connections to our patients is a priority. The focus on heart power has created a patient-centered culture and nurtures the common values of a trusting team focused on the worthy cause of helping each DED patient.
Heart power is also the joy in celebrating the DED victories of our patients. Seeing a patient “get their groove back” (quality of life, biopsychosocial health, work productivity, and family functioning) is the heart and soul of my work as a physician. We don’t give up. Our small, yet mighty, team leans in to create a center dedicated to delivering compassion, healing, and hope for every one of our patients.
Gratitude
In spending my childhood in Montana, I can tell you it takes many helpful and encouraging people to raise a barn. The same is true of a single specialty practice. With hearty gratitude to friends, colleagues, and staff, the success of this comprehensive, advanced, and integrative practice belongs to you as well. I’ll be right over with my proverbial hammer and saw when you call me. Everyone benefits. CP
References:
- Periman LM, Perez VL, Saban DR, Lin MC, Neri P. The Immunological Basis of Dry Eye Disease and Current Topical Treatment Options. J Ocul Pharmacol Ther. 2020;36(3):137-146.
- Periman LM, Mah FS, Karpecki PM. A Review of the Mechanism of Action of Cyclosporine A: The Role of Cyclosporine A in Dry Eye Disease and Recent Formulation Developments. Clin Ophthalmol. 2020;14:4187-4200.









