Once upon a time, dry eye disease (DED) was one of the least well-treated diseases in all of eye care. The Delphi algorithm in 2006 signaled a paradigm shift in addressing this disease.1 Sixteen years later, we have a total of 5 algorithms to aid us in diagnosing and treating DED. All 5 provide excellent guidance for the management of DED. Which one we choose likely depends on the severity of disease we are faced with, and the availability of specialized in-office testing.
Here, I discuss the 3 latest algorithms: Tear Film & Ocular Surface Society Dry Eye Workshop (DEWS II), Corneal External Disease and Refractive Surgery (CEDARS), and ASCRS Cornea Clinical Committee. DEWS II uses a severity-based approach, the CEDARS algorithm is driven by ocular surface disease subtype, and the ASCRS algorithm revolves around presurgical care. The modern algorithms are more similar to one another than not, and all 3 of these share the basic architecture introduced by the Delphi panel. Let’s take a look!
DEWS II
DEWS II is best described as a staged algorithm that divides the DED world into two simple categories: aqueous deficient dry eye (ADDE) and evaporative dry eye (EDE). The diagnostic evaluation begins with a questionnaire (Ocular Surface Disease Index is favorably reviewed), as well as a detailed inquiry about risk factors (e.g., advanced age), external causes (e.g., systemic disease), and medications (e.g., antidepressants). Additionally, point-of-care testing, specifically tear osmolarity and MMP-9 (InflammaDry, Quidel), are included.
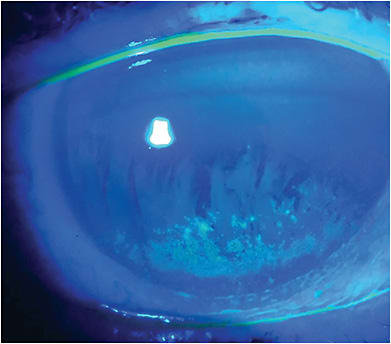
The exam is comprised of lid margin, gland expression, and tear meniscus assessment at the slit lamp. It is suggested that tear break-up time (TBUT) be tested with fluorescein, and staining can be done with any or all the vital dies.2 (Figure 1)
Once a definitive diagnosis is achieved, the options to treat mild-to-moderate disease include dietary supplementation with Omega fatty acids and the use of oil-based artificial tears when addressing EDE.
Additionally, antiinflammatory treatments, such as cyclosporine (Restasis [Allergan/AbbVie] and Cequa [Sun Ophthalmics]) and lifitegrast (Xiidra, Novartis), as well as intense pulsed light are included as options for moderate-to-severe disease.
Punctal plugs are now recommended in Step 2 versus Step 3 in the first DEWS II algorithm.3
CEDARS
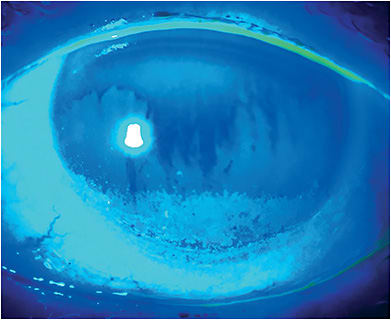
The CEDARS algorithm focuses on the more universal, all-encompassing entity, dysfunctional tear syndrome. Specifically, when seeking to initiate treatment, the algorithm seeks to characterize the disease state in any given patient as classic ADDE, blepharitis or meibomian gland dysfunction (MGD) with or without evaporation, goblet cell abnormality, or exposure. A detailed history and questionnaire are included, and best-corrected visual acuity is evaluated. In-office testing of tear osmolarity and MMP-9 levels are an integral part of the workup, as is Schirmer’s testing with or without anesthesia. Additionally, this algorithm calls for a slit lamp exam with both fluorescein and lissamine green staining of the cornea and conjunctiva (Figure 2). Further tests, such as corneal topography, meibomian gland imaging, and cultures are discussed throughout the publication.4
Once the evaluation is complete, the CEDARS algorithm asks us to determine which of the four disease categories best describes the patient before us, with the understanding that more than one category may coexist, and that each should be addressed. Treatment is linear, beginning with the simplest intervention (e.g., tear supplements) and moving largely in order to more intense or complex treatments (e.g., oral doxycycline/tetracycline) if a given level fails to achieve sufficient resolution of signs and symptoms. The next step would be a subamniotic membrane. If an early-level treatment improves signs and/or symptoms but does not completely resolve them, the next-in-line treatment should be added to the original therapy to augment its beneficial effects.
ASCRS
The ASCRS presurgical algorithm focuses on the quick diagnosis and speedy resolution of DED before cataract and laser refractive procedures, as the condition can cause deleterious outcomes. (See https://bit.ly/3HdMu53 .) Anyone who performs preoperative workups for cataract or refractive surgery will recognize the workflow. The Standard Patient Evaluation of Eye Dryness questionnaire is added to the intake history, and almost all testing (i.e., tear osmolarity, MMP-9, keratometry, topography) takes place before the patient is seen by a doctor. A positive screening (gland imaging, tear film lipid measurement, OCT, higher-order aberrations) sends the patient for additional testing to determine whether the DED is visually significant.5
In addition to what we now know as standard operating procedure for a DED exam — fluorescein staining, TBUT, +/- Schirmer’s testing (“Look” in ASCRS parlance) — the protocol asks us to “Lift” the upper lid to look for floppy eyelid syndrome, “Pull” on the lower lid to uncover signs of conjunctival dysfunction or exposure, and “Push” on the lower lid to evaluate the quality of meibomian gland secretions. (See https://bit.ly/3yV3QAx .) If there is no evidence of DED, the patient proceeds to surgery. If DED is present, but it does not appear to be visually significant (it will neither compromise preop testing nor post-op visual quality), the patient proceeds to surgery.5
Patients who have visually significant DED are referred for treatment along disease-specific pathways that are quite similar to the CEDARS approach. However, since these patients are surgical candidates, the treatment part of the ASCRS algorithm places a premium on a speedy resolution of visually significant DED. Short-term pulse steroid therapy is a primary option, and immunomodulators, such as cyclosporine and lifitegrast, are added if longer term postop dryness is a concern. Treatments reserved for severe disease, such as autologous serum tears and amniotic membrane therapy, are utilized earlier to accelerate resolution of visually significant ocular signs.
Simplifying Care
Every eye doctor who uses a slit lamp is a DED doctor whether or not they choose to admit it. Following one of the algorithms is a simple way to address what is becoming the most frequent diagnosis in all of eye care. CP
References:
- Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006 Sep;25(8):900-907.
- Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575-628.
- The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007 Apr;5(2):75-92.
- Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders–new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;28 (Suppl 1):3-47.
- Starr CE, Gupta PK, Farid M, et al; ASCRS Cornea Clinical Committee. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refractive Surg. 2019;45(5):669-684.









