A 31-year-old male advanced keratoconus (KCN) patient with a history of allergies and constant eye rubbing was referred for corneal transplantation from his local eye care provider. The reason: The patient had failed rigid gas permeable (RGP) and hybrid contact lens wear treatment.
Exam Findings
The patient’s visual acuity measured count fingers at 6 feet OD with no pinhole improvement. OS was 20/30 without correction. Autorefraction showed a refraction of -12.00 + 6.50 x 082 OD and -1.50 + 1.25 x 121 OS. Manifest refraction did not improve OD.
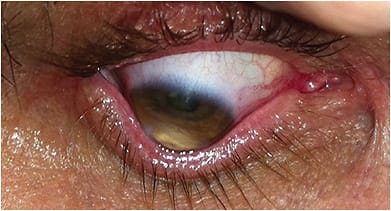
Slit lamp examination revealed extensive apical corneal thinning with no scarring in the right cornea with a prominent Kayser-Fleischer ring and Munson’s sign (Figure 1). Additionally, slit lamp examination showed a clear cornea OS with no obvious apical corneal thinning.
Laying the patient’s chair to a supine position revealed the severity of the cone OD (Figure 2). Tomographic images OD were inaccurate, but manual keratometry values measured 59.5 x 69.5 D. Corneal pachymetry was 375 μm OD and 495 μm OS.

Discussion
While KCN remains one of the most common reasons for keratoplasty across the globe and corneal transplantation has a long track record, dating back to the first successful PK in 1905, improving the vision in advanced KCN without keratoplasty remains a major goal for achieving therapeutic success. Why? Retaining one’s cornea prevents the complications of keratoplasty, such as a suprachoroidal hemorrhage, late traumatic graft rupture, glaucoma and cataracts from topical steroid use, and postoperative infection or rejection. All these complications can potentially lead to complete loss of vision or loss of the eye, even with the best of management (Figure 3).

Something else to keep in mind: Some KCN patients have Pickwickian syndrome, which includes obesity and sleep apnea. These comorbidities make anesthesia and the potential for significant posterior pressure a major concern when needing to perform keratoplasty. On top of those risks is the potential need for a regraft, should graft rejection develop or the keratoconus return decades later, as can happen with corneal transplants that fail to remove all the diseased keratoconic cornea.
The advent of corneal cross-linking (CXL) and scleral contact lenses has allowed for improving the vision in advanced KCN patients without keratoplasty. To start, multiple peer-reviewed publications on CXL have shown the treatment can halt the progression of KCN and flatten the corneal contour.1,2 Additionally, small improvements may be seen in visual acuity, with minimal-to-no complications in CXL.
The initial CXL Epi-OFF technique, often referred to as the Dresden protocol, showed an average decrease in topographic astigmatism of 2.01 D, an average reduction in myopia of 1.14 D, and an improvement in best-corrected vision of 1.26 lines.1 That said, most patients still needed a refractive correction solution to achieve their best vision. (See “Epi-ON CXL and Keratoconus,” below.)
This is where scleral contact lenses come in. They can improve vision beyond RGP lenses, soft lenses, and spectacles; provide protection to the eye while in place; and protect against the perceived most common exacerbating factor for KCN progression in a patient, rubbing the eye.
Specifically, while the lenses are in place, the patient does not have the stimulus to rub the eye, as the lenses increase the moisture around the ocular surface. Lens wear also physically prevents the ability of a patient to rub the eyes while they are being worn. Severinsky and Lenhart found an 83% success rate in the prevention of corneal transplantation and vision improvement in teenagers who had advanced KCN.3 Koppen et al reported on scleral contact lens fitting in patients who had maximal keratometry values over 70 D. A total of 40 out of 51 eyes were able to successfully wear scleral contact lenses with dramatic vision improvement, all while avoiding corneal transplantation.4 Of the 11 cases requiring corneal transplantation, half developed corneal graft rejection.4 These studies underscore the two major advantages of scleral contact lens wear in advanced KCN: Patients can (1) achieve excellent visual acuity and (2) avoid a procedure that carries a lifetime risk of rejection and traumatic graft dehiscence.
Prior to the advent of CXL, patients who had advanced KCN were pigeonholed into needing a therapeutic keratoplasty to remove the diseased ectatic tissue and have it replaced with a large diameter cadaveric donor cornea. Now, if the corneal thickness parameters are appropriate and no significant corneal scarring is present, advanced cases can have FDA-approved CXL followed by scleral lens fitting after 4 weeks, and they can achieve vision recovery without a risky large diameter corneal graft.
EPI-ON CXL AND KERATOCONUS
At present, the only FDA-approved CXL treatment is the Epi-OFF protocol, which was patterned after the Dresden protocol. Studies are ongoing to test the effectiveness of Epi-ON protocols. Additionally, accelerated protocols have been under investigation to see whether adequate results can be achieved in less than 30 minutes using higher UV light fluences than used with the Dresden protocol.
The results of Epi-ON trials and accelerated protocols will ultimately determine whether these technique alterations will have the same duration of treatment as Epi-OFF treatments at 30 minutes of UV light exposure. Epi-ON treatments would certainly be advantageous for the treatment of advanced keratoconus cases, as the corneal thickness parameters could likely be lowered.
Time and additional studies will ultimately determine what is the best technique, but for now we can all agree that avoiding a keratoplasty saves the potential risk for intraoperative hemorrhage, rejection, and graft dehiscence over one’s lifetime.
Management
The 31-year-old male advanced KCN patient was a bouncer at a nightclub, so given the concern for late traumatic graft rupture with a large diameter corneal transplant, it was decided to perform the FDA-approved CXL OD and fit the patient with a scleral contact lens after the corneal surface stabilized to prevent the risks of a cornea transplant related to his current job.
Hypotonic riboflavin was used after the 30-minute riboflavin induction time without difficulty. The patient’s surface normalized with no haze at 4 weeks, and a scleral contact lens fitting was performed at that time.
Outcome
The patient’s uncorrected vision was 20/400 OD, and vision improved to 20/25- OD with the scleral contact lens. This case illustrates that CXL followed by scleral contact lens wear offers the opportunity for successful vision outcomes in advanced KCN patients. CP
References:
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a–induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620-7.
- Seiler TG, Fischinger I, Koller T, Zapp D, Frueh BE, Seiler T. Customized corneal cross-linking: one-year results. Am J Ophthalmol. 2016;166:14-21.
- Severinsky B, Lenhart P. Scleral contact lenses in the pediatric population–Indications and outcomes. Contact Lens Ant Eye. 2021;1:101452.
- Koppen C, Kreps EO, Anthonissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral lenses reduce the need for corneal transplants in severe keratoconus. Am J Ophthalmol. 2018;185:43-47.









