Keratoconus (KCN) screening is important prior to corneal refractive surgery, as laser refractive surgery may lead to accelerated postoperative ectasia in patients who have subclinical signs of KCN.1 Therefore, KCN screening should be a combination of highly sensitive and specific tests to minimize the number of patients mistakenly denied corneal refractive surgery.
The corneal epithelial and stromal thickness profiles may represent this combination. The reason: The corneal epithelium can alter its thickness profile to re-establish a smooth, symmetrical optical outer corneal surface and either partially or totally mask the presence of an irregular stromal surface from front-surface topography.2 Therefore, the epithelial thickness profile would be expected to follow a distinctive pattern in KCN to partially compensate for the cone. Similarly, the stromal thickness profile can provide more sensitive diagnostic information than full corneal thickness analysis because the smoothing effect of the epithelium is removed.
Epithelial thickness mapping aids in the definitive diagnosis of KCN and, in many cases, before there is any detectable corneal front-surface topographic change.
Here, we discuss how to interpret this mapping.
Examining Epithelial Thickness Profiles
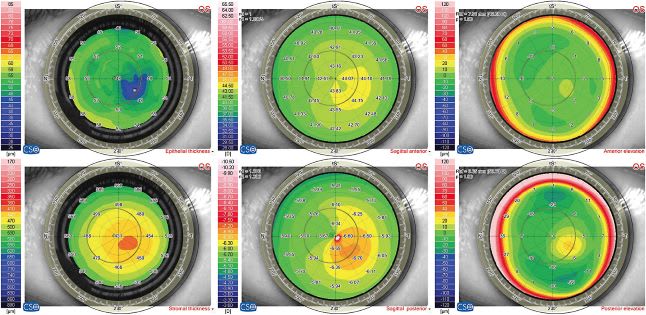
In a population of normal eyes (n=110), the epithelium was 5.7 µm thicker inferiorly than superiorly, and 1.2 µm thicker nasally than temporally, with a mean central thickness of 53.4 µm on average3 (Figure 1). Further, the average central epithelial thickness was 53.4 µm with a standard deviation of 4.6 µm.3 This data indicated little variation in central epithelial thickness in the normal-eye population. The thinnest epithelial point within the central 5 mm of the cornea was displaced on average 0.33 mm (±1.08) temporally and 0.90 mm (±0.96) superiorly with reference to the corneal vertex. Studies using OCT confirm this superior-inferior and nasal-temporal asymmetric profile for epithelial thickness in normal eyes.4

The normal epithelial thickness profile is altered in KCN, as extreme steepening leads to epithelial breakdown, which is often seen clinically. Epithelial thinning over the cone has been demonstrated using histopathologic analysis of KCN corneas by Scroggs et al5 and later using custom software and an OCT system by Haque et al.6 Thus, it is not surprising that the average epithelial thickness profile in KCN revealed significantly more irregularity compared to a normal population.7
Specifically, the epithelium was thinnest at the apex of the cone, and this thin epithelial zone was surrounded by an annulus of thickened epithelium (Figure 1).
While all KCN eyes exhibited the same epithelial doughnut pattern, characterized by a localized central zone of thinning surrounded by an annulus of thick epithelium, the thickness values of the thinnest point and the thickest point, as well as the difference in thickness between the thinnest and thickest epithelium, varied greatly among eyes.7 There was a statistically significant correlation between the thinnest epithelium and the steepest keratometry (D), indicating that as the cornea became steeper, the epithelial thickness minimum became thinner (Figure 2).

Using Epithelial Thickness Profiles
In early KCN, we would expect to see on pachymetry a pattern of localized epithelial thinning surrounded by an annulus of thick epithelium coincident with a suspected cone on tomography scan: posterior elevation best fit sphere (BFS). The coincidence of epithelial thinning together with an eccentric posterior elevation BFS apex may reveal whether to ascribe significance to an eccentric posterior elevation BFS apex occurring concurrently with a normal front-surface topography. So, in the presence of normal or questionable front-surface topography, thinning of the epithelium coincident with the location of the posterior elevation BFS apex would represent total masking or compensation for a sub-surface stromal cone, which does represent KCN. Conversely, finding thicker epithelium over an area of topographic steepening or an eccentric posterior elevation BFS apex would imply that the steepening is not due to a KCN sub-surface stromal cone, but more likely due to localized epithelial thickening. Our study using epithelial thickness profiles had a sensitivity of 99.5% and a specificity of 98.9%.8 If you can exclude KCN, it is safe to proceed with corneal surgery.9
A caveat: Other factors may affect the epithelial pattern. Epithelial changes associated with anterior basement membrane dystrophy (ABMD) may cause focal areas of a thickening that can be identified on slit-lamp. In addition to ABMD, the epithelium can also be affected by dry eye disease, which can cause overall epithelial thickening, but often result in an irregular or asymmetric pattern.
Abnormal eyelid anatomy can also induce significant changes to the epithelial thickness profile (Figure 3).
For example, in a patient who has a ptosis, the superior epithelium becomes thinner due to the constant pressure of the eyelid. Thus, it is important to consider the epithelial thickness profile in the context of the clinical exam; an abnormal epithelial thickness profile should prompt a thorough check for these possible explanatory symptoms.
Another Diagnostic Method
KCN detection is evolving. We have demonstrated in this article that the epithelial thickness profile was significantly different between normal eyes and KCN eyes. The epithelial thickness profile also progresses along with the evolution of KCN. The distinctive epithelial doughnut pattern associated with KCN can be used to confirm or exclude the presence of an underlying stromal surface cone in cases of normal or suspect front-surface topography, as well as being a “qualifier” for the finding of an eccentric posterior elevation BFS apex.
With continued advancements in KCN screening, combining the measurements from multiple diagnostic techniques and devices, we can better serve those patients interested in corneal refractive surgery. CP
References:
- Ambrosio R Jr, Wilson SE. Complications of laser in situ keratomileusis: etiology, prevention, and treatment. J Refract Surg. 2001;17(3):350-379.
- Reinstein DZ, Archer T. Combined Artemis very high-frequency digital ultrasound-assisted transepithelial phototherapeutic keratectomy and wavefront-guided treatment following multiple corneal refractive procedures. J Cataract Refract Surg. 2006;32(11):1870-1876.
- Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness in the normal cornea: three-dimensional display with Artemis very high-frequency digital ultrasound. J Refract Surg. 2008;24(6):571-581.
- Li Y, Tan O, Brass R, Weiss JL, Huang D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology. 2012;119(12):2425-2433.
- Scroggs MW, Proia AD. Histopathological variation in keratoconus. Cornea. 1992;11(6):553-559.
- Haque S, Simpson T, Jones L. Corneal and epithelial thickness in keratoconus: a comparison of ultrasonic pachymetry, Orbscan II, and optical coherence tomography. J Refract Surg. 2006;22(5):486-493.
- Reinstein, DZ., Gobbe, M., Archer, T., Silverman, R., Coleman, J. Epithelial, stromal and total corneal thickness in keratoconus. J Refract Surg. 2010 Apr;26(4):259-71.
- Silverman RH, Urs R, Roychoudhury A, Archer TJ, Gobbe M, Reinstein DZ. Epithelial remodeling as basis for machine-based identification of keratoconus. Invest Ophthalmol Vis Sci. 2014 Mar 13;55(3):1580-7.
- E.g. Reinstein DZ, Archer TJ, Gobbe M. Stability of LASIK in topographically suspect keratoconus confirmed non-keratoconic by Artemis VHF digital ultrasound epithelial thickness mapping: 1-year follow-up. J Refract Surg. 2009 Jul;25(7):569-77.










