Dry eye disease (DED) may be considered a disease of modern living. Specifically, current generations contend with causes, such as screen time, contact lenses, and extensive beauty and personal hygiene routines. Furthermore, we live longer than previous generations did — we know advanced age is a risk factor for DED — and the Western diet isn’t exactly healthy. Another important consideration is that clinicians and patients are finally paying attention to this problem, which today affects over 16 million Americans.1
The ancient Chinese word Dao means “way” or “path.” In my practice, I’ve developed an approach to treating DED and other ocular surface disorders (OSDs) that I call the DAO: an acronym for addressing the Dermatologic, the Aesthetic, and the Ophthalmologic aspects of eye care. The DAO is a Venn diagram-like approach that borrows from other subspecialties to illustrate what’s happening on the ocular surface and to enable our patients to have healthier, more beautiful, and more comfortable eyes.
Here, I discuss these individual aspects:
Dermatological Aspects
As clinicians, we tend to exclusively zero in on the ocular surface using the slit lamp. However, we really need to look at what’s happening in the entire neighborhood around the eyes, as the neighborhood can have a direct effect on the health of the ocular surface.
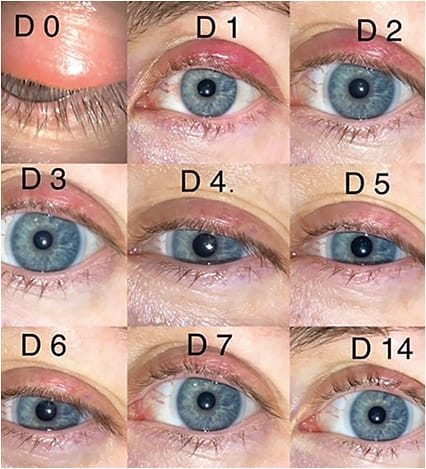
For example, it is important for clinicians to examine the skin for evidence of rosacea. The reason: An estimated 80% of rosacea patients suffer from meibomian gland dysfunction (MGD), a leading component of ocular surface disease.2 Learning to recognize the signs of rosacea early can be very helpful in the successful treatment of OSDs (Figure 1). Typical findings may include eyelash changes, telangiectasias, lid thickening, lid edema, MGD, conjunctivitis, keratitis, and neovascular scarring in severe cases.

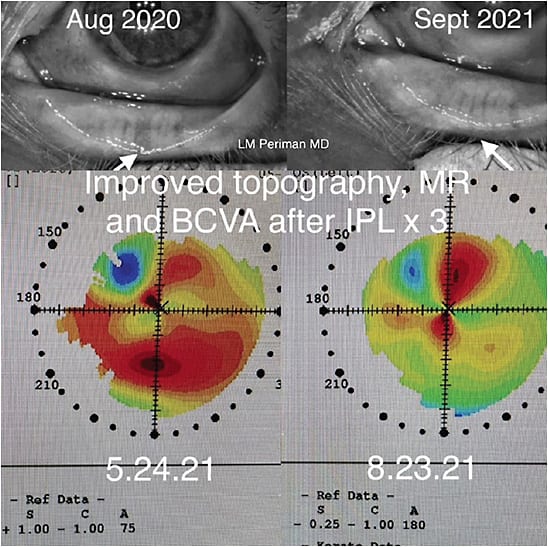
When I have a DED patient who is showing early signs of ocular or facial rosacea, I suggest intense pulsed light (IPL) treatment. IPL is widely used by dermatologists as a noninvasive treatment for a wide variety of skin conditions that ophthalmologists can use to help manage MGD associated with DED.
I find that a series of 4 to 6 in-office treatments is effective — you’ll see excellent improvement in meibum quality. Patients say they appreciate the improvement in their skin’s appearance as well. Other effective treatments for MGD include warm compresses, lid hygiene, topical antibiotics, anti-inflammatories, thermal treatments, meibomian gland probing, lipid-containing artificial tears, in-office heat and expression therapies, and manual or mechanical microblepharoexfoliation.
Another troublesome skin condition is seborrheic dermatitis, which affects the scalp, eyelids and eyebrows, as well as other areas where sebaceous glands are located. The condition causes red skin, scaly patches, and persistent dandruff. Like rosacea, seborrheic dermatitis can play a role in MGD3 (Figure 2). Seborrheic dermatitis responds well to prescription ketoconazole shampoo and ketoconazole cream. Additionally, I offer an IPL treatment series to patients who have this condition, as I have found it to be effective (Figure 3).

A caveat: If you see something you’re not sure about, send the patient for a consultation with a dermatologist. This is especially important when you’re just getting started in this area and still developing your clinical experience and knowledge base. Something else to keep in mind: Lupus-like rash needs systemic evaluation and coordination with rheumatology. Morbihans syndrome is characterized by significant non-pitting edema and erythema of the face. The more we collaborate with and understand the overlap of subspecialties, the better the outcomes for the patient.
Aesthetic Aspects
Many clinicians do not discuss cosmetics and beauty topics with their patients4 (Figure 4). However, anyone concerned about OSD has noticed the very real health costs associated with everyday beauty and hygiene practices by patients. Therefore, the products and treatments commonly used by both women and men should be discussed by the eye care provider. After all, beauty can turn ugly when it comes to ocular health.

Let your patients know that products deemed “good” for their facial skin are not necessarily good for their eyes. Even the mildest face cleansers can strip the delicate meibum that protects the corneal tear film. To avoid this, let patients know that the eye area needs special hygiene agents, such as commercial eyelid wipes, and hypchlorous acid. Their face wash should not be used to clean their eyelids or remove their makeup.
Something to consider: There is marked confusion about the ocular surface impact of retinol (vitamin A) and its derivatives. Studies have shown that the acne drug Accutane (isotrenotin) is associated with MGD and lacrimal dysfunction.5 However, vitamin A in ophthalmic ointment form is helpful for the ocular surface; while cis-retinoic acid and cis-retinoic acid receptors are important for maintaining ocular surface integrity.5
Commonly repeated advice around waterproof makeup avoidance also may or may not be true for the dry eye patient.3 Waterproof makeup is a potential friend and enemy for the dry eye disease patient. As a friend, having a stay-put formula that does not smear with artificial tear use, is desirable. However, the artificial stiffening of the eyelashes and the difficulty in removing waterproof makeup may counteract any potential gains.
Cosmetics preservatives are very important to prevent fungal and bacterial contamination. Underpreserved eye makeup products are associated with serious infections. However, certain preservatives commonly found in cosmetics can be very hard on the ocular surface. Two specific categories of preservative to avoid for ocular surface disease patients are formaldehyde-donating preservatives (i.e., sodium hydroxymethylglycinate, quaternium-15, DMDM hydantoin, and ureas) and benzalkonium chloride (BAK). Two other categories of preservatives, parabens and phenoxyethanol, require a more nuanced analysis. At low concentrations, these preservatives do not demonstrate cell death in culture.7 Furthermore, parabens are very effective preservatives and rarely cause cases of allergic dermatitis.8
The ideal makeup remover does not overstrip the meibum, does not introduce BAK, chelating agents, ethylene diamine tetra-acetic acid, and does not contain tear film destabilizing ingredients.
Argireline (acetyl hexapeptide-3 or acetyl hexapeptide-8) is sometimes touted as “Botox in a jar” because it eliminates wrinkles by relaxing facial muscles. However, Argireline products applied around the eyes may weaken the orbicularis oculi muscle, affecting both the ability to blink and to express meibum.
That’s not to say that patients can’t use cosmetic injections and procedures. If done properly, injections of Botox (Allergan) can be a DED friend.9 Conversely, Botox should be avoided in the crow’s feet in DED patients, as well as in those at risk for this condition. Studies have shown that Botox injections into the crow’s feet negatively impact Schirmer scores in an age-dependent fashion.10 This may be due to the uptake of neurotoxin in the lacrimal gland, which negatively impacts tear production.
Botox can be effective in treating conditions, such as filamentary keratitis and superior limbic keratoconjunctivitis (SLK). A few years ago, I came across a research paper from Gumus et al, who injected a few units of Botox right above the lashes in the superior orbicularis muscle of filamentary keratitis patients. After the initial injection, 88% of the treated eyes had total resolution in the filaments.11 I use a modification of this technique for my filamentary keratitis and SLK patients to reduce friction between the lid wiper and the bulbar conjunctiva, which provides relief from that sandpaper feeling with each blink.
A few years ago, I was part of a team that developed a survey intended to identify relationships between cosmetic use habits and ocular surface disorders. We found that respondents who did not remove their makeup had higher SPEED scores than those who did.12 However, makeup removers may be loaded with some of the problematic ingredients previously described.
Ophthalmic Aspects
The final element of the Venn diagram-like approach focuses on ophthalmologic treatment, which can include nutrition recommendations, omega fatty acid supplementation, artificial tears, inflammation control, and in-office treatments. (See “Reviewing In-Office Dry Eye Disease Treatments,” at bit.ly/InOfficeDED .)
Good nutrition is a vitally important component of good eye health. I’m a believer in omega fatty acid supplementation. But supplements aren’t enough if the patient isn’t eating properly.
Studies have shown that rosacea patients often suffer from reduced gut microflora biodiversity, which may increase gut and body-wide inflammation.13
My rosacea patients’ most common dietary triggers are wheat and dairy. I often recommend a nutrition program called the Whole 30 to these patients. There’s an online platform (https://whole30.com ), a bestselling book, and patients can sign up for related newsletters. The Whole 30 program enables patients to better understand their physical responses (bloating, constipation, diarrhea, acne, rosacea flares, joint pain, etc.) to certain foods.
Some of your patients may suffer from sleep apnea, which is more common in males than females.14 Sleep apnea is a commonly overlooked contributor to OSD. (See “Sleeping Devices Awaken Dry Eye,” at bit.ly/CPAPOSDCP .) The chronic inflammation induced by nightly hypoxic episodes is responsible for the development of floppy eyelid syndrome.15 CPAP machines address this nightly hypoxic injury, and eyelid hyperlaxity may slowly improve with continued use.16 The flip side is that CPAP masks can leak turbulent air, which can dry out the ocular surface. To address this, I suggest that CPAP users wear an eye mask or special disposable stickers during sleep.
Recent innovations and studies regarding artificial tears, as well as experience with clinical trials, have convinced me of the value of artificial tears. In fact, recent research revealed that lipid-based artificial tears are associated with improvements in symptoms of tear stability, staining, and improved meibomian gland secretion scores.17
The prescription anti-inflammatory tool kit includes steroids, as well as the immunomodulators cyclosporine and lifitegrast. In a 2021 study, cataract surgery patients who had DED showed significant improvement in symptoms and refractive accuracy after b.i.d. treatment with topical cyclosporine 0.09% drops (Cequa; Sun Ophthalmics) for 28 days.18 Another recent study of 100 eyes concluded that b.i.d. treatment with lifitegrast 5% (Xiidra; Novartis) significantly improved preoperative corneal surface measurement accuracy in patients who had confirmed DED and who were scheduled for cataract surgery.19 Restasis (Allergan), Klarity-C (Imprimis Pharmaceuticals) and generic Restasis (Mylan Pharmaceuticals, Inc.) are also immunomodulators.
Bringing it All Together
As you can see, there is a lot of overlap among the dermatologic, aesthetic, and ophthalmic aspects of care.
Taking a holistic approach shows patients that you care deeply for them as people and want to see them thrive by modifying their everyday habits and daily chemical exposures to reduce inflammation. CP
References:
- Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90-98.
- Viso E, Clemente Millán A, Rodríguez-Ares MT. Rosacea-associated meibomian gland dysfunction—an epidemiological perspective. Eur Ophthal Rev. 2014;8(1):13-6.
- Yasar E, Kemeriz F, Gurlevik U. Evaluation of dry eye and meibomian gland dysfunction with meibography in seborrheic dermatitis. Cont Lens Anterior Eye. 2019;42(6):675-678.
- Periman LM. Understanding ocular surface irritation potential from mascara products in the dry eye disease patient: a microscopic analysis of multiple products. Paper presented at: American Society of Cataract and Refractive Surgery (ASCRS) annual meeting; April 22-26, 2022; Washington, D.C.
- Yeh, T. Effects of Isotretinoin on Meibomian Glands. Dissertation. University of California at Berkeley; 2019. Accessed April 29, 2022. https://escholarship.org/uc/item/3mm9k54s
- Alam J, Yu Z, de Paiva CS, Pflugfelder SC. Retinoid regulation of ocular surface innate inflammation. Int J Mol Sci. 2021;22(3):1092.
- Periman LM, Maiti S. Cosmetics and tear film inflammation. Video presented at: Eyes on Dry Eye 2022 virtual conference; March 15, 2022.
- Favoretto Cordeiro AC, Salvador BC, Szpak R, et al. Allergic contact dermatitis after the use of cosmetics containing parabens: systematic review and meta-analysis. Braz Arch Biol Technol. 2022;65: e22210377.
- Horwarth-Winter J, Bergloeff J, Floegel I, Haller-Schober EM, Schmut O. Botulinum toxin A treatment in patients suffering from blepharospasm and dry eye. Br J Ophthalmol. 2003 Jan;87(1):54-6. doi: 10.1136/bjo.87.1.54.
- Gunes A, Demirci S, Koyuncuoglu HR, Tok L, Tok O. Corneal and tear film changes after botulinum toxin-a in blepharospasm or hemifacial spasm. Cornea. 2015;34(8):906-910.
- Gumus K, Lee S, Yen MT, Pflugfelder SC. Botulinum toxin injection for the management of refractory filamentary keratitis. Arch Ophthalmol. 2012;130(4):446-50.
- O’Dell LE, Periman LM, Sullivan AG, Halleran CC, Harthan JS, Hom MM. An evaluation of cosmetic wear habits correlated to ocular surface disease symptoms. Ophth Vis Sci. 2017;58:ARVO
- Daou H, Paradiso M, Hennessy K, Seminario-Vidal L. Rosacea and the microbiome: a systematic review. Dermatol Ther (Heidelb). 2021;11(1):1–12. Published online 2020 Nov 10.
- Mohsenin V. Effects of gender on upper airway collapsibility and severity of obstructive sleep apnea. Sleep Med. 2003;4(6):523-9.
- Schlötzer-Schrehardt U, Stojkovic M, Hofmann-Rummelt C, Cursiefen C, Kruse FE, Holbach LM. The pathogenesis of floppy eyelid syndrome: involvement of matrix metalloproteinases in elastic fiber degradation. Ophthalmology. 2005;112(4):694-704.
- Vieira MJ, Silva MJ, Lopes N, Moreira C, Carvalheira F, Sousa JP. Prospective evaluation of floppy eyelid syndrome at baseline and after CPAP therapy. Curr Eye Res. 2021;46(1):31-34.
- Craig JP, Muntz A, Wang MTM, et al. Developing evidence-based guidance for the treatment of dry eye disease with artificial tear supplements: A six-month multicentre, double-masked randomised controlled trial. Ocul Surf. 2021;20:62-69.
- Hovanesian JA, Berdy GJ, Epitropoulos A, Holladay JT. Effect of cyclosporine 0.09% treatment on accuracy of preoperative biometry and higher order aberrations in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2021;15:3679-3686.
- Hovanesian J, Epitropoulos A, Donnenfeld ED, Holladay JT. The effect of lifitegrast on refractive accuracy and symptoms in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2020;14:2709-2716.









