Topography-guided custom ablation treatment (TCAT) can be a handy tool in the refractive surgeon’s armamentarium, with potential use in both routine cases and atypical eyes. In contrast to wavefront-guided ablation, which plans treatment utilizing aberrations of the entire optical system (including both cornea and lens), TCAT incorporates aberrations from the anterior cornea and is centered on the corneal vertex. Patients treated with TCAT may achieve excellent visual and aberrometric outcomes.1 That said, as is the case with all ophthalmic surgeries, the likelihood of a successful outcome is contingent on patient selection.
Here, we discuss important characteristics of TCAT candidates.
Pristine Preoperative Topography
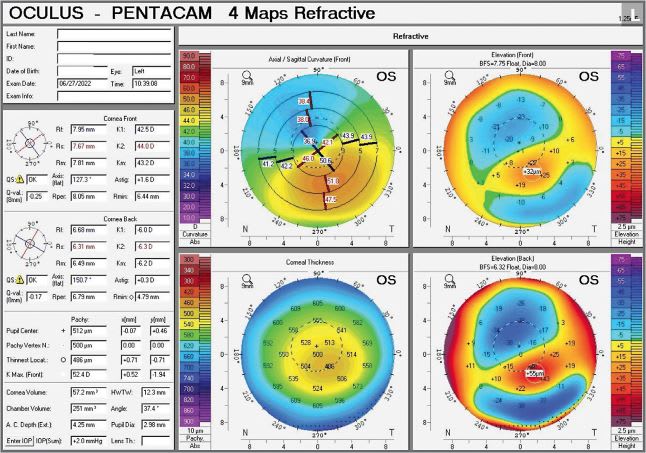
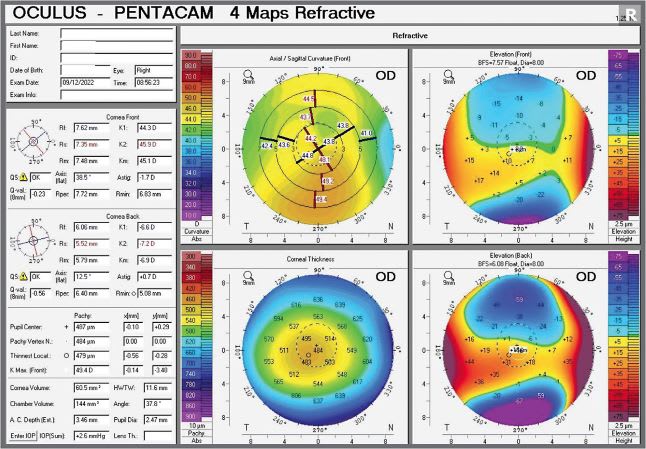
A critical criterion for TCAT candidacy is good-quality, consistent, and repeatable preoperative topography.2,3 Poor data quality input results in poor quality output for the treatment. At least 4, and, preferably, 6 to 8 preoperative topographic maps are recommended to perform TCAT to ensure internal consistency of the preoperative measurements.2-4 If TCAT is felt to be well-suited to the patient, but the quality of preoperative topography is limited by ocular surface disease, such as dry eye disease, then the ocular surface should be treated, and measurements repeated to reassess TCAT candidacy.4
Patient Expectations
Realistic patient expectations are also important in selecting TCAT candidates. Treatment utilizing TCAT may require a staged approach to achieve reliable refractive outcomes, especially in more irregular corneas. In a staged approach, the goal of the initial treatment is primarily corneal normalization (with varying amount of refractive treatment), and a subsequent treatment is sometimes anticipated to achieve the final refractive goal. Should the initial corneal normalization procedure seem unlikely to achieve a good refractive outcome and a staged approach is anticipated, the refractive surgeon should clearly communicate to the patient about the need for multiple procedures. If a patient who has an irregular cornea has unrealistic expectations for a “one and done” result, that patient may be a poor TCAT candidate.
Older Age
Some refractive surgeons have suggested older age (e.g., age over 50 years) as a criterion for selecting TCAT candidates, as younger patients, in whom cataract surgery is less imminent, might benefit additionally from treatment of lenticular aberrations using wavefront-guided approaches.3 We consider age to be a soft criterion, which is, perhaps, most applicable to routine refractive candidates.
Myopic Refractive Error
TCAT is FDA approved for the treatment of up to -9.00 D of myopic spherical equivalent, with up to -8.00 D of myopia, and up to -3.00 D of astigmatism.5 As higher-order aberrations (HOAs) may originate at an irregular corneal surface, using TCAT in primary refractive procedures provides an opportunity for not only improving acuity, but improving quality of vision through reduction of HOAs.3
To this effect, some refractive surgeons might consider all patients undergoing routine myopic refractive surgery to be candidates for TCAT if the treatment falls within the treatable limits of TCAT. A more targeted approach within the FDA-approved indication might be to selectively utilize TCAT in routine primary refractive cases that also have slightly irregular corneas. In other words, these are patients who would benefit from both refractive treatment and corneal reshaping.
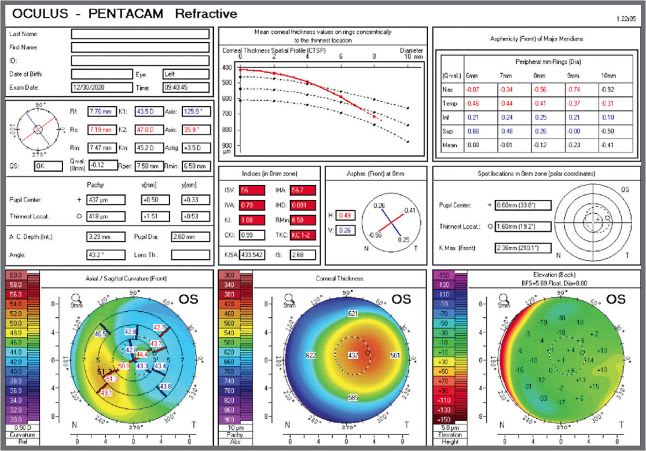
Additional good candidates are those who have significant HOAs who may not get optimal vision from glasses or contact lenses. Most refractive patients have HOAs less than 0.3 mm and refractive surgeons have historically considered total HOAs over 0.4 mm (which represents 3% to 5% of refractive candidates) to be visually significant, while and 0.3 mm was considered borderline. Now, with more experience with topography-guided treatments, and results of clinical trials, one should consider TCAT for treatment of over 0.3 mm and often lower, depending on specific aberrations, such as coma.
Previous Refractive Surgery Complications
TCAT may be utilized off-label as an attempted refractive salvage procedure in eyes that have complications from previous refractive surgery. Specifically, TCAT provides an opportunity for simultaneously addressing higher-order aberrations caused by corneal irregularities, as well as improving visual outcomes.6 To this effect, TCAT has been reported for use in the enhancement of eyes that have decentered ablations,6-9 small ablation zones,6-7 and irregular astigmatism after previous laser refractive surgery.6,10,11
Highly Aberrated Irregular Corneas
Another off-label usage of TCAT is the normalization of highly aberrated or irregular corneas.2 This group of TCAT candidates includes post-keratoplasty eyes,12,13 postradial keratotomy (RK) eyes,14 and eyes that have keratoectasia (including postrefractive surgery ectasia15). When TCAT is used for corneal normalization in irregular or highly aberrated corneas, it can be performed as a single procedure or in a staged approach, preceding cataract surgery or additional keratorefractive surgery, to improve final refractive outcomes.
Several studies have revealed favorable outcomes for TCAT after keratoplasty12,13 and after RK.14 Bizrah et al reported long-term efficacy, safety, and stability in 54 eyes of 50 patients who underwent either previous PKP or deep anterior lamellar keratoplasty and were treated with topo-guided photorefractive keratectomy (PRK).13 Ghoreishi et al reported a series of transepithelial PRK after previous RK, with improvement in both corrected and uncorrected visual acuity, as well as reduction in HOAs, spherical aberration, and coma.14
Patients who have keratoectasia, including both keratoconus (KCN) and postrefractive surgery ectasia, may also be candidates for TCAT, depending on the severity of their disease. For example, patients who have stable mild-to-moderate ectasia, can be considered for corneal normalization, including for improving contact lens fit.15,16 However, it is important to keep in mind that ablation in keratoectasia patients carries the risk of worsening their keratoectasia, so patients should be counseled accordingly.15
Patients who have progressive KCN or postrefractive surgery ectasia may also benefit from TCAT as a sequentially staged procedure performed after corneal cross-linking (CXL). Specifically, the stages can be performed using an intervening recovery period, but they can also be performed immediately sequentially on the same day, commonly referred to as the Athen’s protocol.15,17,18
Incidentally, there is now 10-year follow-up data for the Athen’s protocol in progressive KCN, demonstrating its long-term stability, safety, and efficacy.19 Investigation of the Athen’s protocol for postrefractive ectasia is smaller and doesn’t yet have as long of follow-up, but also supports a role for immediately sequential CXL and TCAT in postrefractive surgery ectasia.20
Consider TCAT
TCAT may provide favorable visual, refractive, and aberrometric outcomes in well-selected candidates, as described above. TCAT does have its risks, including undesired spherical refractive outcome, and ectasia.
The refractive surgeon can consider using TCAT as a primary refractive procedure, an enhancement in eyes that have complications from previous refractive surgery, and for the normalization of irregular or highly aberrated eyes. Further long-term follow-up data and experience with TCAT will help refine algorithms for selecting candidates. CP
References:
- Zhang Y, Sun X, Chen Y. Comparison of corneal optical quality after SMILE, wavefront-optimized LASIK and topography-guided LASIK for myopia and myopic astigmatism. Front Med (Lausanne). 2022;9: 870330.
- Ramamurthy S, Soundarya B, Sachdev GS. Topography-guided treatment in regular and irregular corneas. Indian J Ophthalmol. 2020;68(12): 2699-2704.
- Nattis A, Rosenberg E, McDonald M, Donnenfeld ED. Topography-guided ablations: early US experience and utility across the refractive landscape. Curr Ophthalmol Rep. 2017;5: 232-238.
- Pasquali T, Krueger R. Topography-guided laser refractive surgery. Curr Opin Ophthalmol. 2012;23(4): 264-268.
- United States Food & Drug Administration. Premarket Approval (PMA), Allegretto Wave Eye-Q Excimer Laser System. United States Food & Drug Administration website. October 23, 2013. Accessed August 9, 2022. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P020050S012
- Shetty R, Lalgudi VG, Kaweri L, et al. Customized laser vision correction for irregular cornea post-refractive surgery. Indian J Ophthalmol. 2020;68(12): 2867-2879.
- Lin DT, Holland SR, Rocha KM, Krueger RR. Method for optimizing topography-guided ablation of highly aberrated eyes with the ALLEGRETTO WAVE excimer laser. J Refract Surg. 2008;24(4): S439-S445.
- Kymionis GD, Panagopoulou SI, Aslanides IM, Plainis S, Astyrakakis N, Pallikaris IG. Topographically supported customized ablation for the management of decentered laser in situ keratomileusis. Am J Ophthalmol. 2004;137(5): 806-811.
- Wu L, Zhou X, Ouyang Z, Weng C, Chu R. Topography-guided treatment of decentered laser ablation using LaserSight’s excimer laser. Eur J Ophthalmol. 2008;18(5): 708-715.
- Chen X, Stojanovic A, Zhou W, Utheim TP, Stojanovic F, Wang Q. Transepithelial, topography-guided ablation in the treatment of visual disturbances in LASIK flap or interface complications. J Refract Surg. 2012;28(2): 120-126.
- Alió JL, Belda JI, Osman AA, Shalaby AM. Topography-guided laser in situ keratomileusis (TOPOLINK) to correct irregular astigmatism after previous refractive surgery. J Refract Surg. 2003;19(5): 516-527.
- Spadea L, Visioli G, Mastromarino D, Alexander S, Pistella S. Topography-guided trans-epithelial no-touch photorefractive keratectomy for high irregular astigmatism after penetrating keratoplasty: a prospective 12-months follow-up. Ther Clin Risk Manag. 2021;17: 1027-1035.
- Bizrah M, Lin DTC, Babili A, Wirth MA, Arba-Mosquera S, Holland SP. Topography-guided photorefractive keratectomy for postkeratoplasty astigmatism: long-term outcomes. Cornea. 2021;40(1): 78-87.
- Ghoreishi M, Peyman A, Koosha N, Golabchi K, Pourazizi M. Topography-guided transepithelial photorefractive keratectomy to correct irregular refractive errors after radial keratotomy. J Cataract Refract Surg. 2018;44(3): 274-279.
- Hatch KM, Ling JJ, Wiley WF, et al. Diagnosis and management of postrefractive surgery ectasia. J Cataract Refract Surg. 2022;48(4): 487-499.
- Shetty R, D’Souza S, Srivastava S, Ashwini R. Topography-guided custom ablation treatment for treatment of keratoconus. Indian J Ophthalmol. 2013;61(8): 445-450.
- Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol). J Refract Surg. 2014;30(2): 88-93.
- Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9): S812-S818.
- Kanellopoulos AJ. Ten-year outcomes of progressive keratoconus management with the Athens Protocol (topography-guided partial-refraction PRK combined with CXL). J Refract Surg. 2019;35(8): 478-483.
- Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens Protocol. J Refract Surg. 2011;27(5):323-331.










