Researchers have recently reported that keratoconus (KCN) is more common than previously thought. Specifically, the condition affects nearly 4 million people around the world, based on a conservative prevalence estimate of one case per 2,000.1
Because keratoconus can progress to permanent vision loss, it’s essential that eye care providers are aware of the latest sight-preserving interventions.
Here, I discuss the range of intervention options.
Spectacles
In its early stages (corneal curvature less than 45 D) and mild forms, KCN can be corrected with spectacles alone.
With increasing corneal irregularity from KCN, however, glasses become ineffective at correcting vision.
Contact Lenses
Certain contact lens options can aid in correcting KCN-associated higher-order aberration distortions, as they have different cylinder power and axis requirements than spectacles. These contact lenses include:
- Standard soft toric contact lenses. These contact lenses often provide some level of improvement in patients who have mild or early KCN, as toric contact lenses have thick profiles, offering some correction. That said, these contact lenses commonly produce unreliable powers in patients who have irregular astigmatism, so an optimal prescription for these patients requires proper over-refraction after the contact lenses have settled on the eyes.
- Soft specialty contact lenses. New, soft specialty contact lenses have been specifically designed for KCN patients. One has a steep, central base curve and a flat outer curve that conforms to the sclera’s curvature. Another utilizes aspheric optics to optimize vision for KCN patients. These are just two examples.
- Rigid gas-permeable (RGP) contact lenses. The rigid surface of these small-diameter contact lenses can correct irregular astigmatism and higher-order aberrations caused by abnormal corneal shape, making them ideal for patients who have central cones.First-time RGP users may experience lens awareness, which requires a period of adaptation. I have found that most patients are able to adapt to these contact lenses.
- Hybrid contact lenses. These contact lenses provide RGP optics in the center and a soft skirt around the edges, providing patients with both good vision and comfort. Hybrids contact lenses are effective for patients who have improved vision with RGP lenses but experience discomfort or dislodging of the lens.
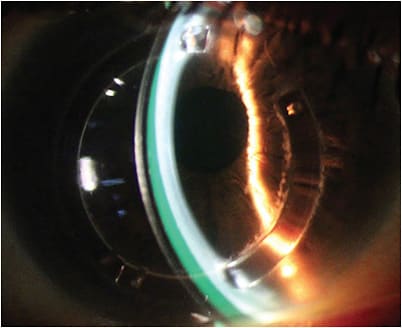
- Scleral contact lenses. These large-diameter RGP CLs vault the cornea, lying directly on the conjunctiva overlying the sclera and creating a tear reservoir that can mask the irregular corneal surface. Thus, they can reduce or neutralize higher-order aberrations and decrease lower-order aberrations caused by the eyes themselves. Additionally, they have a large optical zone, which can result in enhanced vision. One scleral lens is filled with preservative-free saline.Successful scleral lens fit depends on three important factors: (1) a proper central corneal vault, between 100 μm and 300 μm; (2) an appropriate limbal clearance; and (3) a landing zone no steeper or flatter than the scleral profile.

Intracorneal Ring Segments
Intracorneal ring segments are small, arc-shaped implants of varying thickness and length made of inert plastic. They are implanted in a laser-cut channel within the cornea.
Their purpose is to provide a gross shape correction in moderate to advanced KCN in which vision is poor due to corneal shape irregularity.
Corneal Cross-Linking
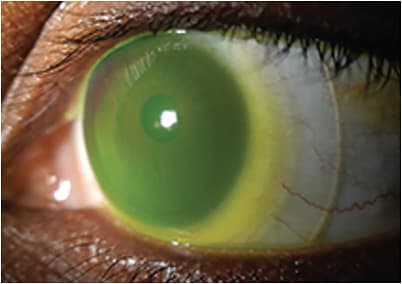
Patients who have severe corneal irregularities typically will be unable to achieve functional acuity using the options discussed above, as they can’t correct the distortion caused by KCN-associated higher-order aberrations (e.g., glare, ghosting, and starbursts). This is where corneal cross-linking (CXL) comes in.
CXL arrests the progression of corneal ectasia by regularizing corneal shape via an epithelium-off (or epi-OFF) procedure or an epi-ON procedure. The former has FDA approval and is designated to treat patients who have progressive KCN and post-LASIK ectasia, using the Dresden protocol. The latter does not have FDA approval.
The Dresden protocol consists of debriding the central corneal epithelium and loading the corneal stroma with photosensitizer via riboflavin 5-phosphate ophthalmic solution at 2-minute intervals for 30 minutes. Debriding the epithelium allows for the riboflavin to infuse the corneal stroma.
From there, ultraviolet-A light photoactivates the riboflavin, creating oxygen radicals in the corneal stroma, which cause permanent collagen cross-links to form.
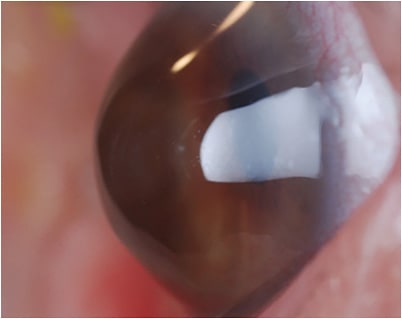
Postoperatively, patients are prescribed corticosteroids and topical antibiotics. To facilitate re-epithelialization and provide optimal comfort to the eye, a sterile bandage contact lens is applied after CXL.
In the early follow-up period, epi-OFF CXL patients are treated similarly to those who have undergone a photorefractive keratectomy procedure. Complete re-epithelialization is the first step toward long-term healing. Within the first postoperative month, symptoms of recovery typically include a drop or fluctuation in patients’ best spectacle-corrected visual acuity, which usually returns to baseline within 3 months.
Additionally, topographies and tomographies often show reductions in keratometry readings, followed by gradual stabilization (6 to 12 months).
The complications associated with the epi-OFF procedure include postop pain, which decreases with every passing day; keratitis (sterile or infectious); delayed epithelial haling, which can lead to persistent epithelial defect/corneal melt; corneal edema; corneal opacity; and endothelial damage.
The epi-ON procedure leaves the epithelium intact during riboflavin absorption into the stroma. Thus far, this has been accomplished with chemical additives in the riboflavin solution, an increased concentration of riboflavin, an extended amount of time in riboflavin application, topical anesthetic application, partial epithelial disruption, and iontophoresis.
To facilitate healing, these patients are prescribed corticosteroids and topical antibiotics. They may or may not be fitted with a bandage contact lens.
The rare but possible complications linked with the epi-ON procedure are foreign body sensation, which is expected to resolve within 24 hours after the operation, and transient photophobia and hyperemia.
A Recipe for Success
It is important to identify KCN early to preclude patient behaviors, such as eye rubbing, which can exacerbate the condition’s progression. Incidentally, atopy and allergy are strongly associated with KCN, as both conditions cause patients to rub their eyes.
When KCN patients have concomitant atopic conditions, it’s important to encourage them to use cool compresses and appropriate pharmacotherapy, such as topical mast cell stabilizer/antihistamine combinations, in conjunction with corticosteroids to achieve relief, and to discourage them from rubbing their eyes.
Early identification of KCN coupled with access to the latest interventions may prevent the need for corneal transplantation. CP
Reference:
- Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101(3):267-273.









