Corneal cross-linking (CXL) has been a game changer for our corneal ectasia patients. Specifically, the procedure, available in both epi-OFF (FDA approved in 2016) and epi-ON (off-label) can maintain vision in these patients by halting further corneal thinning, which can preclude the need for keratoplasty.
Here, I review the innovations and complications of CXL.
Riboflavin Solution
Initially, many surgeons used dextran-diluted riboflavin for the procedure. When it was discovered that dextran-diluted riboflavin dehydrated and thinned the cornea significantly intraoperatively, saline-diluted riboflavin, which holds the promise of readily being able to diffuse to the cornea stroma, and not cause significant dehydration, was employed. Avedro introduced a higher-concentration riboflavin solution, VibeX, VibeX Rapid, as well as VibeX Xtra and ParaCel, which contain riboflavin solutions. The first is of higher concentration, and the later contains special preservatives to dissolve epithelial cell bonds and facilitate the large riboflavin molecule to penetrate intact epithelium easier for transepithelial treatments.
Of note: Iontophoresis, a technique pioneered in Italy, uses a mild electric current to draw the larger riboflavin molecules into the corneal stroma and accelerates its bioavailability.
In 2007, I was part of a team that introduced the concept of administering riboflavin within a corneal pocket, created by a femtosecond laser. There are several investigators who have worked on and are working on proprietary riboflavin solutions. Oxygen supplementation is an adjunct application.
Protocols
I have long practiced the Athen’s protocol CXL technique. This consists of preceding the accelerated CXL procedure by a partial-in refraction, essentially “minimal” thickness reshaping for the ectasia surface ablation, which, in essence, is a topographic-guided ablation to normalize the corneal surface, removing up to 50 μm of corneal stroma from the cone area that usually is the thinnest. This enhances the bioavailability of the riboflavin solution in the corneal stroma within minutes after its administration and reduces soaking time to just 5 minutes after the PTK procedure. Then, accelerated CXL at, 6 mW/cm2 for a total of 15 minutes is used to deliver a similar amount of energy of 5.4 J to the cornea to establish effective CXL, documented by a very deep (70% to 80%) and homogeneous CXL line of 9 mm diameter, seen clinically and on anterior segment OCT.
Various other protocols exist for the epi-OFF procedure, including oxygen supplementation during the procedure, as noted above, under the auspice that it will accelerate further the CXL photochemical reaction that may become titrated from the lack of oxygen at some point.
The epi-ON (leaving the epithelial on) CXL protocol introduces the riboflavin molecule within the corneal stroma and has been shown to reduce the morbidity of the epithelial defect that causes significant patient discomfort, a longer visual rehabilitation, and the potential of more complications and longer time exposed to the potential of infectious keratitis.
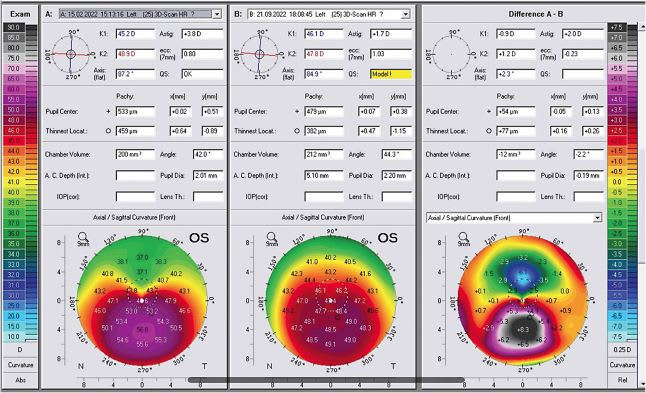
In refractive CXL, a different pattern and different fluence, UV light that is customized through corneal topography or cornea pachymetry maps, can attain not only stabilization of the cornea but also a controllable refractive effect. This procedure, the refractive CXL, has been CE-marked in the European Union since 2013 and has had some success in becoming an alternative refractive procedure for small refractive errors. It is currently under investigation by several centers internationally, though not yet FDA approved.
Potential Complications
Known complications of CXL are cornea melt, infectious keratitis, significant corneal haze, and more than desired rigidity in the cornea, including non-homogeneous “hardening” of the cornea that can cause significant refractive changes.
I was part of a team that recently reported on the 10-year experience with the Athen’s protocol in a large number of patients. Specifically, we saw that in a small percentage of cases, under 2%, progressive flattening may occur over the years, and that should be taken into account when refractive planning is considered in these patients.
Nevertheless, when known and dealt with properly, these complications are minor compared to cornea transplantation. Specifically, if a patient was contact lens intolerant and had poor spectacle acuity, inevitably a PKP was the treatment of choice. Now, a small fraction of these patients undergo this procedure.
What’s to Come?
Outside the United States, CXL is approved for refractive corrections and we have reported since 2013 some of the first cases. CXL is also used as an adjunct to PRK and/or LASIK, or intracorneal ring segment surgery. Further, several protocols are under investigation internationally for its use for infectious keratitis, as well as for corneal edema.
U.S. ophthalmologists often ask, “Can the Dresden CXL protocol be optimized to increase its applicability across various clinical scenarios?” There is not a definitive answer. Since its introduction, the Dresden protocol has been altered significantly.
In 2005, my team introduced higher fluence CXL, initially 5m W, then 7 mW, then 10 mW/cm2, as presented at the pre-Academy ICRS meeting in 2007. Several investigators followed along with the industry to reach levels up to 30 mW/cm2, and named higher-fluence CXL: “accelerated CXL.” Among the different protocols, most mainly deliver similar total amount of total energy (usually with difference fluence) close to the 5.4 J that the Dresden protocol addresses. When fluence is increased, the treatment is shorter and, thus, called accelerated. We have yet to see extensive controlled prospective comparative studies on the subject. CP









