How I treated a mass of possible destruction
Welcome to “My Corneal Save,” a new magazine department that provides a firsthand account of a memorable cornea case and how the ophthalmologist was able to help the patient.
A 68-year-old Puerto Rican male presented reporting a progressive decrease in vision in his left eye over the last year. He said he first noticed a growth on the same left eye roughly 2 years ago that had been getting progressively larger.
Additionally, the patient reported bloody discharge from the growth, intermittent ocular irritation, and that he had been having difficulty opening his left eye. The rest of his medical and ocular history, along with his lifestyle, were unremarkable. The patient had light skin pigmentation, and said he spent most of his adult life outdoors.
Exam Findings
Initial exam revealed a spectacle-corrected visual acuity of 20/40 in the right eye and 20/250 in the affected left eye.
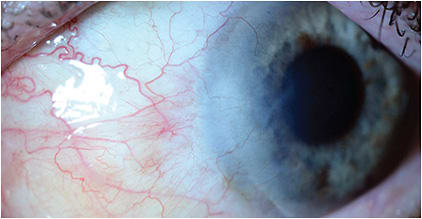
Slit lamp exam of the left eye was remarkable for an 8.5 mm (v) by 11.5 mm (h) elevated interpalpebral nasal conjunctival lesion that extended into the nasal cornea (Figure 1).

The view into the anterior chamber was limited, but the pupil was round, and there were no signs of intraocular inflammation.
View to the fundus was also limited, but the posterior segment exam appeared normal, without signs of a posterior lesion.
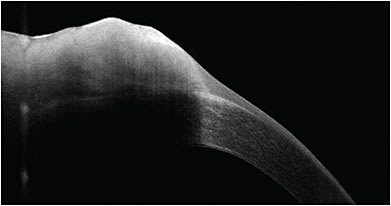
OCT of the lesion was performed. It revealed a thickened hyperreflective epithelium with an abrupt transition from normal epithelium (Figure 2).
There were no signs of intraocular extension of the lesion, but given its size, ultrasound biomicroscopy was performed to determine whether there was any scleral invasion. Unfortunately, resolution in the area of concern was limited, so a definitive answer regarding whether this lesion invaded through the basement membrane could not be ascertained.
Of note: Impression cytology and confocal microscopy are additional modalities that can be used to evaluate neoplasms of the conjunctiva.
Diagnosis
Clinical exam results were highly suggestive of ocular surface squamous neoplasia (OSSN), given the elevated nasal conjunctival lesion located within the intrapalpebral fissure, the lesion’s thickened hyperreflective epithelium on OCT, and the patient’s years of exposure to ultraviolet radiation, due to his outdoor lifestyle.
OSSN is a spectrum of malignancy that ranges from mild conjunctival intraepithelial dysplasia (CIN) to invasive squamous cell carcinoma (SCC). CIN is a slow-growing tumor localized to the epithelial layer and confined by an intact basement membrane. SCC occurs when neoplastic cells penetrate the basement membrane and extend into the substantia propria. The term corneal epithelial dysplasia is used to describe neoplastic lesions that are exclusively or predominantly found in the cornea that have minimal conjunctival involvement.
An important risk factor for OSSN is excessive UV light exposure, which damages cellular DNA and affects the tumor suppressor TP53 gene. Additional risk factors include cigarette smoke exposure, immunodeficiency (including HIV infection), light skin, HPV, petroleum product exposure, and xerophthalmia.
Management
Until 2022, a popular treatment option for OSSN was interferon alpha-2b. This is an immunomodulatory cytokine that was available as a topical drop or a sub-conjunctival injection for the treatment of OSSN. Interferon alpha-2b is no longer being manufactured and is currently not available as a treatment for OSSN in the United States.
The treatment options for OSSN in the United States are now surgical excision with wide margins and cryotherapy, or topical chemotherapy.
Surgical excision places patients at risk for conjunctival scarring, symblepharon formation, and limbal stem cell deficiency. The reported recurrence rate of OSSN following surgical excision ranges from 5% to 56% in cases in which the surgical margins were positive.1 In these cases, topical chemotherapy, discussed next, or radiation can be considered. (To see what surgery entails, visit https://eyewiki.aao.org/Ocular_Surface_Squamous_Neoplasia .)
Topical chemotherapy, available in 2 treatments stateside, allows for the treatment of the entire ocular surface, making it an option to treat both large and small lesions. The 2 available treatments in the United States today:
1. 5-Fluorouracil (5-FU). This is a pyrimidine analogue solution that impairs DNA synthesis and halts the proliferation of neoplastic cells. The most common side effects are conjunctival injection and superficial punctate keratitis. The reported recurrence with 5-FU is between zero and 28%.2
My regimen for OSSN treatment is 5-FU 1% dosed q.i.d. for 1 week, followed by a 3-week break. The adjuvant use of preservative-free artificial tears and topical steroids can make the treatment more tolerable. Patients are counseled they will likely need several cycles until the lesion resolves, at which point I typically tackle with 1 or 2 additional cycles to treat any residual neoplastic cells that remain after macroscopic clinical resolution.
2. Mitomycin C (MMC). This is a DNA alkylating agent that inhibits mitosis and must be refrigerated. MMC is available in 2 concentrations: 0.02% or 0.04%. Its side effects are ocular pain, possible limbal stem cell loss, and corneal epithelial toxicity, which becomes more pronounced as the concentration increases. MMC treatment is also cycled with 1 week of q.i.d. treatment, followed by 3 weeks off treatment, due to side effects. Several cycles are often needed until the lesion resolves. There are several different ways to dose this. I prescribe 0.04% and cycle it 1 week on and 3 weeks off because of the side effects. Some other regimens are 2 to 4 weeks.
Given the extensive size of the patient’s lesion and the potential uncertainty and morbidity of surgical excision, the decision was made to start with topical chemotherapy. The expectation was the patient would need to undergo several cycles of treatment. A total of 5 cycles were administered.
Outcome
The patient had a tremendous positive response to treatment. At the end of 5 cycles, there were no clinical signs of OSSN on slit lamp examination of the cornea and conjunctiva (Figure 3). Additionally, repeat OCT of the area was performed, and the conjunctival and corneal epithelium appeared normal without any areas of thickening or hyperreflectivity. CP
References:
- Shields CL, Chien JL, Surakiatchanukul T, Sioufi K, Lally SE, Shields JA. Conjunctival tumors: review of clinical features, risks, biomarkers, and outcomes—The 2017 J. Donald M. Gass Lecture. Asia Pac J Ophthalmol (Phila). 2017;6(2):109-120.
- Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol. 2013;24(4):336-42.









