Contact lenses can enable many patients to avoid corneal surgery long term. Even in the setting of successful surgery, 10-year graft survival rates for full-thickness corneal grafts range from 59% to 80%.1 Additionally, it is estimated that 53% of patients worldwide have access to corneal transplantation.2 Further, surgical intervention poses risks, such as infection, bleeding, pain, scarring or failure with the need to repeat surgical intervention. For these reasons, it makes sense for ophthalmologists to take into consideration the conservative management of corneal disease using contact lenses prior to contemplating corneal surgery. That said, it’s important to remember that long-term treatment with contact lens wear also has risks, such as dry eye disease (DED), corneal abrasion, corneal ulcer, or corneal neovascularization. The bottom line: It is important to weigh all potential risks when discussing treatment options.
Here, I discuss the specific types of contact lenses that can be used to effectively manage corneal disorders, and the specific disorders than can benefit from each type.
Soft
Soft contact lenses are made from flexible material that rests over the corneal surface. This flexible material often allows for improved patient comfort with wear and is frequently used as bandage contact lenses for this reason.

• Specific corneal disorders that can benefit. Ocular surface disease (OSD) can be challenging to manage for eye care providers, as there is no single therapeutic regimen for treatment.
Most patients have multifactorial causes for their OSD and require an individualized approach for management.
A multitude of disorders may cause OSD, including evaporative or aqueous-deficient DED. As soft contact lenses can be more accessible and can cost less than some other forms of contact lenses, often providers may alter the materials and oxygen permeability of these contact lenses to facilitate comfort in DED patients.
Ocular surface diseases often require lifelong treatment and repeated surgical interventions. The goal of OSD treatment is to maintain a lubricated ocular surface to avoid the complications and surgical interventions that carry significant risk and long-term morbidity for patients.
Soft contact lenses are preferred over other contact lens types for OSD when treating non-healing corneal epithelial defects, as these contact lenses provide more comfort due to their thin profile. Additionally, soft contact lenses provide a consistent barrier to the trauma from blinking and allow for corneal epithelialization and avoidance of surgical interventions, such as tarsorrhaphy.
Due to their flexibility, soft contact lenses tend to drape over irregularities in the cornea. For this reason, they are not good options for significant corneal irregularities, such as keratoconus or irregular astigmatism, after corneal transplant.
Rigid Gas Permeable
Rigid gas permeable (RGP) contact lenses allow for oxygen transmission to the cornea, thus deeming them “gas permeable.” Additionally, RGP contact lenses provide high-quality vision, and are less likely to dry out compared to soft contact lenses. They rest over the corneal surface with a thin layer of tear film between. RGP contact lenses have a small diameter and do not extend past the corneal limbus.
• Specific corneal disorders that can benefit. RGP contact lenses can mask irregularities within the cornea due to an RGP’s rigid material. Thus, RGP contact lenses are often utilized in cases of corneal irregularity from epithelial basement membrane dystrophy or mild ectasia, such as mild keratoconus.
RGPs are more difficult to use in cases of severe corneal irregularity, such as severe keratoconus or ectatic corneal grafts, as the smaller diameter of RGP contact lenses may allow for movement that can cause discomfort or decentration in these cases.
Corneal grafts, such as a deep anterior lamellar keratoplasty and a penetrating keratoplasty, can cause irregular astigmatism from suture tension or a recurrence of ectasia within the graft over time. RGP contact lenses may work to treat these, as they are often easier for patients to insert versus a larger contact lens, such as a scleral contact lens. Proper fitting may allow patients to avoid re-grafting due to irregular astigmatism.
Hybrid
Hybrid contact lenses utilize an RGP lens in its center with a small skirt of soft contact lens material around its diameter. These contact lenses allow patients to combine the best properties of both RGP and soft contact lenses by increasing comfort and quality of vision.
• Specific corneal disorders that can benefit. Hybrid contact lenses may be a good alternative for patients who have corneal disease and cannot otherwise tolerate RGP contact lenses. These contact lenses can be tried for patients who have epithelial basement membrane dystrophy or mild keratoconus and experience discomfort or decentration with RGPs.
Scleral
Scleral contact lenses are large in diameter and rest on the scleral surface, providing a vault over the corneal surface. This vault allows for a fluid cleft between the contact lens and cornea.
Specific subtypes of scleral contact lenses may be customized to fit the size and shape of varying irregularities of the ocular surface. These contact lenses offer ocular surface masking and support due to their significant vault.
Additionally, scleral contact lenses provide added patient comfort in some cases, as they do not rest directly on the corneal surface.
• Specific corneal disorders that can benefit. Scleral contact lenses can be utilized as a supportive treatment for a wide range of mild-to-severe corneal pathologies. These contact lenses may be selected for patients who have DED and have become intolerant to soft contact lenses, as scleral contact lenses maintain a consistently lubricated ocular surface and avoid touching the cornea.
Scleral contact lenses are often preferred in severe ocular surface disease, such as graft-versus-host disease, Stevens-Johnson syndrome, chemical burns, mucous membrane pemphigoid, neurotrophic keratopathy, and exposure keratopathy. These severe disorders carry a long-term risk of limbal stem cell deficiency that may cause photophobia, epithelial defects, and irregular astigmatism. These conditions are more easily managed using a scleral contact lens, as the vault can be altered to support corneal stability and spare the corneal limbus from further damage and avoidance of limbal stem cell transplantation.3 In some cases of persistent epithelial defects, scleral contact lenses may be partially filled with antibiotic to avoid risks, such as microbial keratitis.
Corneal scars causing irregular astigmatism may also be managed with scleral contact lenses. This is particularly the case in patients who have OSD as a cause for corneal scarring: Scleral contact lenses provide both continuous lubrication for the corneal surface, as well as mask irregular astigmatism. These contact lenses support the underlying disease process, as well as visual rehabilitation to avoid high-risk corneal grafting.
Scleral contact lenses have been successfully utilized in cases of exposure keratopathy and persistent epithelial defects by providing a corneal fluid barrier to allow for epithelialization,3 therein avoiding the need for surgical intervention, such as tarsorrhaphy.
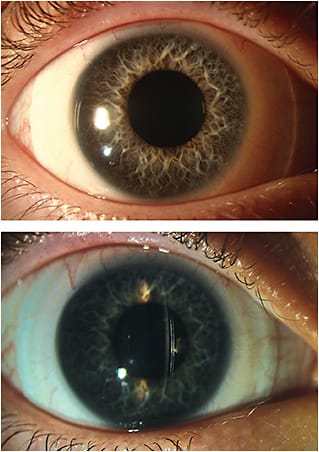
Inherited corneal dystrophies, keratoconus, postrefractive ectasia or pellucid marginal degeneration can cause severe corneal irregularity. In these cases, often RGP or hybrid lenses cannot provide enough vault over the cornea to mask the irregular astigmatism caused by these disorders.
Additionally, ectatic disorders can result in corneal scarring, which may further impede the patient’s ability to see clearly. The SCOPE study noted that scleral contact lenses were prescribed for ectasia in 74% of patients.4 Scleral contact lenses are often preferred over RGP or hybrid contact lenses in these cases, as they provide reduction of astigmatism and higher-order aberrations, allowing for avoidance of corneal transplantation. For the same reason, scleral contact lenses are also a great option for patients who have already undergone keratoplasty. Scleral contact lenses are often needed post-transplantation, particularly when patients are dissatisfied with the lack of comfort or degree of visual improvement from RGP or hybrid contact lenses.
Remember Contact Lenses
Recent innovations in contact lens technology have allowed many patients the option of pursuing contact lens wear prior to consideration of surgery. Furthermore, many patients can avoid surgery long term when successfully fit with a contact lens.
A caveat: Each treatment regimen must be considered on an individual basis, and all risks associated with treatment should be presented to patients before a treatment decision is made. CP
References:
- Price MO, Thompson RW, Price FW. Risk factors for various causes of failure in initial corneal grafts. Arch Ophthalmol. 2003; 121(8): 1087-92.
- World report on vision. World Health Organization. October 8, 2019. Accessed May 24, 2023. https://www.who.int/publications/i/item/9789241516570
- Harthan JS, Shorter E. Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations. Clin Optom (Auckl). 2018; 11(10): 65-74.
- Nau CB, Harthan J, Shorter E, et al. Demographic characteristics and prescribing patterns of scleral contact lens fitters: The SCOPE study. Eye Contact Lens. 2018; 44: S265-72.









