Granular corneal dystrophy type 2 (GCD2) can result in significant eye discomfort and vision loss. (See “GCD2: An Overview”) The good news: Surgery can remove as many opacities as possible to resolve the symptoms without compromising the structural integrity of the cornea.
Options for surgery include deep anterior lamellar keratoplasty (DALK), superficial keratectomy, phototherapeutic keratectomy (PTK), or a full-thickness penetrating keratoplasty (PK). (See “Performing Penetrating Keratoplasty Remains Essential,” p.18) These surgeries are effective against GCD2 because they target the layer of corneal tissue that has the most corneal deposits.
Here, we discuss 3 patients who underwent 3 different surgeries for their GCD2.
Case 1:
Difficulty Driving at Night
A 48-year-old male presented with complaints of glare and trouble driving at night. His Snellen uncorrected visual acuity was 20/200 in the right eye and 20/60 in the left eye. His best-corrected visual acuity (BCVA) was 20/60 in the right eye and 20/40 in the left eye. Glare testing revealed decreased vision to light perception in the right eye and 20/200 in the left eye. His medical history was otherwise unremarkable.
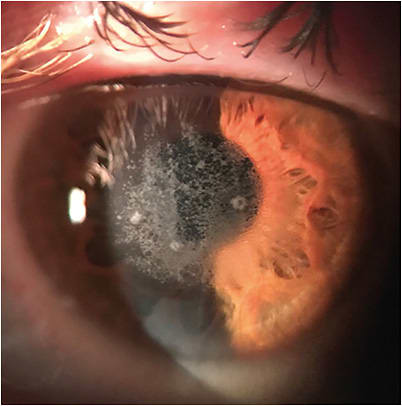
Examination showed granular deposits in the anterior stroma of both corneas (Figure 1) consistent with GCD2. An anterior-segment (AS)-OCT of the right eye revealed granular and hyaline deposits throughout the anterior and mid stroma. AS-OCT is paramount for determining the depth of granular deposition in the cornea.

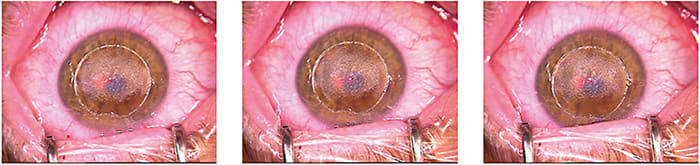
Due to the depth of the deposits, the patient underwent an uncomplicated DALK, and had complete resolution of his stromal opacities (Figure 2). Histopathology confirmed granular and hyaline deposits in the diseased corneal specimen consistent with GCD2.

The patient’s vision is now 20/70 uncorrected in the right eye and 20/40 uncorrected in the left eye, with resolution of his glare. Additionally, all corneal sutures have now been removed, and he has been fitted with a scleral contact lens that has increased his vision to 20/20 with a clear graft and complete resolution of granular dystrophy.
His left eye showed significantly less hyaline deposition in the mid stroma, but a majority in the superficial stroma and epithelium (Figure 3). Despite less deposits compared to the treated right eye, the left eye had recurrent corneal erosion symptoms, including constant pain, redness, and discomfort upon waking.

Case 2:
Like Father, Like Daughter
The daughter of the patient in Case 1 initially presented at age 15 with bilateral corneal deposits similar to her father that were consistent with GCD2, in terms of appearance.
She was brought in for a routine examination due to her father’s diagnosis. The patient did not have complaints initially. Medical and ocular history were otherwise unremarkable. At the time of this visit, she had mild subepithelial granular deposits with concomitant irregular epithelium in both eyes (Figure 4).

Her best-corrected Snellen visual acuity (BCSVA) was 20/20 in both eyes. Given these findings, the patient was monitored with serial annual examinations.
Over time, she started developing mild recurrent erosion symptoms like her dad, and was prescribed lubricant tears to be used 3 to 4 times a day. The tear use resulted in resolution of the recurring irritation of both eyes for the next 3 years during her annual routine checkups.
The patient presented recently with complaints of unbearable foreign body sensation, worse in her left eye—suspicious for worsening recurrent corneal erosions. AS-OCT showed subepithelial deposits that had minimal stromal involvement (Figure 5).

She underwent a superficial keratectomy of the left eye with diamond burr polishing. The procedure is shown to reduce recurrent corneal erosion symptoms and worked well in her dad’s case.
The patient has reported resolution of her recurrent corneal erosion symptoms, and her vision has remained stable with 20/20 BCSVA. Her right eye is stable with minimal symptoms, so the patient deferred any surgical intervention on this eye.
Case 3:
Post-LASIK Glare and Halos
A 45-year-old male presented complaining of glare and halos. His ocular history was positive for uncomplicated LASIK, which he underwent 5 years previously. His BCVA was 20/30 OD and 20/40 OS. Medical and ocular history was otherwise unremarkable.
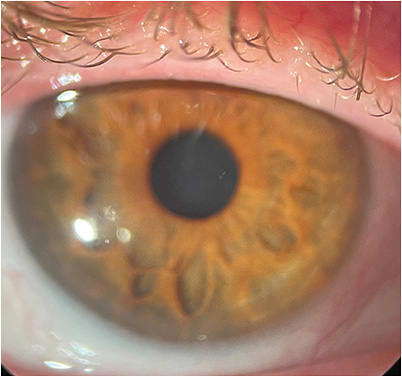
Examination showed superficial central granular deposits in the left eye worse than what appeared in the right eye (Figure 6). AS-OCT revealed the deposits were concentrated in the LASIK flap and the anterior portion of the flap bed.
A genetic analysis showed the patient was heterozygous for the TGFB1 R124H allele, which is consistent with GCD2. Of note: Refractive procedures are contraindicated in patients who have GCD2, as these procedures can rapidly increase the rate of hyaline deposition in the cornea.1,2 Thus, patients who have unexplained corneal opacities should undergo genetic testing for corneal dystrophies before considering any elective corneal surgeries.
Due to the superficial nature of the granular opacities, the patient elected to proceed with flap amputation and phototherapeutic keratectomy to the stromal bed. The flap was amputated, and an excimer laser was used to ablate the cornea to a target of -3.00 D, followed by an immediate second treatment to a target of +3.00 D to sufficiently ablate the subsurface opacities (Figure 7). Of note: If the deposits are located exclusively along the interface, the flap can be lifted, and the posterior flap and bed could be ablated without amputation in such patients.3
GCD2: AN OVERVIEW
GCD2 is inherited in an autosomal dominant fashion. It was first described in 1988 in 4 patients from 3 families who traced their origins to Avellino, Italy.
The condition is caused by a mutation in the transforming growth factor beta-induced gene (TGFBI), which leads to deposition of hyaline and amyloid in the epithelium, superficial-stroma, and mid-stroma.
Symptoms that drive patients to the eye doctor are recurrent corneal erosion symptoms of redness, irritation, and eye pain, or decreased vision.
Clinically, GCD2 presents with 3 signs that can cause glare, limit vision, and lead to recurrent corneal erosions:
- Anterior stromal gray-white granular deposits with clear intervening spaces.
- Midstromal lattice lesions.
- Anterior stromal haze.4
The differential diagnosis of bilateral corneal opacities include granular dystrophy type 1 or lattice corneal dystrophy. The appearance of the lesions is often helpful in making a diagnosis but genetic testing is the definitive method for confirmation of the diagnosis based on the type of genetic mutation present.
Mitomycin C was applied to the cornea for 30 seconds. The patient’s epithelium healed without complication, and his postop VA was 20/25 uncorrected at month 1, with reports of excellent improvement in his glare symptoms (Figure 8). At month 4, the patient developed superficial haze, which is currently being treated with topical steroids and cyclosporine. The patient underwent the same procedure in the right eye without complication, and can now see 20/20 in this eye without correction.
Picking the Procedure
If deposits are anterior, superficial keratectomy or PTK should be performed. The choice between the two must be made by the corneal surgeon.
If deposits involve the mid and posterior stroma, DALK or PK should be considered, with again, the choice between the 2 at the discretion of the corneal surgeon. However, corneal transplants have a higher rate of complication, may require lifelong contact lens use, and can fail multiple times over a patient’s lifetime. Therefore, if the ophthalmologist believes most opacities are anterior enough and the patient’s visual symptoms can be minimized with a superficial procedure, this should be considered first-line treatment. If symptoms persist after a superficial procedure, a DALK or PK can always be completed secondarily. CP
References:
- Woreta FA, Davis GW, Bower KS. LASIK and surface ablation in corneal dystrophies. Surv Ophthalmol. 2015;60(2):115-122.
- Lee WB, Himmel KS, Hamilton SM, et al. Excimer laser exacerbation of Avellino corneal dystrophy. J Cataract Refract Surg. 2007;33(1):133-138.
- Kim TI, Hong JP, Ha BJ, Stulting RD, Kim EK. Determination of treatment strategies for granular corneal dystrophy type 2 using Fourier-domain optical coherence tomography. Br J Ophthalmol. 2010;94(3):341-345.
- Holland EJ, Daya SM, Stone EM, et al. Avellino corneal dystrophy. Clinical manifestations and natural history. Ophthalmology. 1992;99(10):1564-1568.









