Since the modern invention and further development of endothelial keratoplasty (EK) procedures, penetrating keratoplasty (PK) procedures have declined. In 2005, PK represented 95% of all transplants according to the Eye Bank Association of America Annual Statistical Report.1 As of 2021, PK represented 33% of all corneal transplants performed in the United States, with EK becoming the most common type of corneal transplantation.2 Regardless of this reduction, PK remains an essential procedure for the surgeon to perform, as EK cannot resolve all corneal opacities.
Conditions affecting the corneal stroma, such as chronic graft rejection, traumatic scars, infectious corneal melts, and stromal corneal dystrophies, must be repaired with a PK rather than an EK. Therefore, PK has not become a lost art, but rather transcends time. (See: “PK: A Brief History,” below.)
In this article, I highlight the clinical scenarios in which the classic PK procedure remains essential for the cornea transplant surgeon, and I discuss the importance of patient education before moving forward with the procedure.
Indications for PK
• Cornea transplant failure. This is the most common indication for PK.2 Specifically, chronic keratoplasty failure often leads to stromal scarring and haze, which cannot be surgically repaired with an EK. Furthermore, prior PKs for keratoconus (KCN) can have recurrence in the graft, revealing severe ectasia, which requires repeat PK. Of note: If the PK has failed and visual acuity was acceptable with limited astigmatism prior to the graft failure, along with absence of stromal scarring or haze, one can attempt EK under the PK graft.
• End-stage KCN. KCN in its end stages can lead to Descemet’s membrane (DM) ruptures, hydrops, and apical scarring. Performing a successful deep anterior lamellar keratoplasty (DALK) in the setting of a prior DM rupture is often quite challenging. Hydrops cases have DM scarring in the visual axis, which can limit vision if a DALK is performed. Also, the air bubble injection step of a big-bubble DALK leads to air escaping from the cornea into the anterior chamber, forming a rupture of DM. This makes the surgery unsuccessful. The PK procedure works best in eyes that have had prior hydrops for these reasons.
While corneal cross-linking (CXL) has forever changed the treatment algorithm for KCN, and, as a result, surgeons hopefully see the need for transplantation for this condition subside as the years go on, it is important to remember that CXL can halt disease progression but not reverse damage or disease.
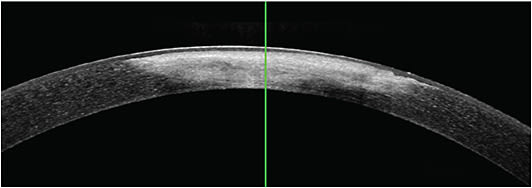
• Corneal scarring and stromal opacity. EK cannot treat stromal scarring and disease. Successful PK is contingent on clinically assessing the degree to which stromal opacities and scars truly limit the best-corrected visual acuity (BCVA) for each patient. (OCT imaging of the cornea can aid surgeons in determining the depth and density of stromal scars.) This assessment can result in 20/40 BCVA or better. Therefore, I generally recommend a PK in situations in which BCVA is less than 20/40.3
PK: A BRIEF HISTORY
The first PK was performed by Dr. Eduard Zirm in 1905 to help treat a patient who had severe alkali corneal burns. For many years, PKs were performed using enucleated eyes from living donors. This persisted until modern eye banking was established and cornea procurement from cadavers was standardized.
As a related aside, I recommend pursuing more conservative treatments, such as hard contact lens wear or phototherapeutic keratectomy (PTK) to help improve VA when possible, due to the intensive recovery and commitment required of patients when undergoing a PK. If OCT imaging confirms the scar is superficial (less than 100 µm), PTK can be a useful adjunct to remove scarring and provide better cornea clarity, allowing the chance to avoid the increased risk involved with PK compared to PTK. Hard contact lenses represent another alternative to surgery and can improve VA greater than one would expect in the setting of a dense stromal scar.
Recently, I had a patient who was left with a soft contact lens-induced paracentral dense stromal scar that extended into the visual axis from a healed corneal infection. VA improved from 20/200 Snellen acuity to 20/25 after fitting with a rigid gas permeable (RGP) contact lens.
• Mechanical trauma and corneal perforation. Traumatic corneal scars represent another corneal problem irreparable with an EK procedure. Due to the nature of the stroma and violation of the DM from these issues, PK is required in these cases. Traumatic scars that are full thickness, involve the visual axis, and induce poor vision despite RGP contact lens wear are cases appropriate for PK.
In my practice, corneal gluing can often be a temporizing measure to see whether the cornea can heal under the glue patch. Multiple repeat glue applications may be required for a cornea to finally heal, but it can be done. However, the risk of infection cannot be underestimated, and I do not recommend delaying surgery in the setting of a brisk wound leak that cannot be tamponaded with glue.

Rarely, infectious keratitis can lead to corneal perforation and an emergent PK must be performed. PK in this setting carries a poor prognosis due to the high risk of rejection and failure or recurrence of the infection. Uncontrolled infectious keratitis from bacteria, fungi, herpetic infections or Acanthamoeba can often lead to repeat infection in the new graft, despite the use of intracameral antibiotics and antifungal medications at the time of surgery. I have often used a glue patch, doxycycline, and vitamin C in cases of severe stromal thinning in the setting of infectious keratitis to stave off perforation.
• Bullous keratopathy. While this is now primarily treated with EK, chronic edema due to the condition can lead to stromal haze and scarring. The combination of endothelial dysfunction and stromal opacification necessitates PK. Neither EK nor DALK can provide success in these situations, which underscores the importance of a prompt referral, so that an EK can be performed before it is too late. PK is the end-stage solution. If referral is made sooner, than PK can be avoided.
• Corneal stromal dystrophies. Many corneal stromal dystrophies can be treated with DALK. The more common dystrophies include corneal dystrophies type 1 and 2 (see “Deterring Corneal Dystrophy Type 2,” p.28), lattice corneal dystrophy, and macular corneal dystrophy. Surgeons who have not learned DALK may still treat these dystrophies with a PK. While PK has an increased risk of endothelial rejection and higher intraoperative complication risk, not all surgeons have DALK in their surgical armamentarium.
• Congenital corneal opacities. Congenital corneal opacities requiring PK are the least common of the conditions mentioned in this article. These opacities may result from conditions, such as sclerocornea or Peters anomaly. Additionally, scars may result from severe congenital ocular infections related to bacteria and herpes simplex virus. Any opacity not corrected quickly in a newborn or toddler will lead to amblyopia. Management of these cases with a pediatric ophthalmologist are paramount for decision making and amblyopia management if a PK must be performed in these clinical scenarios.
After reading these indications for PK, surgeons may be asking, “Why perform PK, when DALK can be performed? After all, it avoids the intraoperative risks of open-sky surgery (suprachoroidal hemorrhage, damage to intraocular structures, etc.), and it eliminates the possibility of endothelial rejection.” Fair question. The answer: DALK certainly is a satisfactory option for several of these indications for PK, but it also has some inherent hurdles. These include a steep learning curve, lack of exposure to DALK in most accredited cornea and external disease fellowships, and potential complications, such as interface haze, interface keratitis, double anterior chamber, intraoperative DM perforations, and stromal/epithelial rejection.4
Patient Education
Despite the long-term success of PK, it remains important to educate patients on the level of commitment involved in undergoing PK: The recovery time is slow, the surgery carries more risk, compliance with drops and follow-up visits are critical, and postoperative complications remain higher than EK surgery. Patients must be aware of these issues, so they are not surprised and, therefore, dissatisfied with their choice to undergo PK. Observation remains an important alternative for many patients.
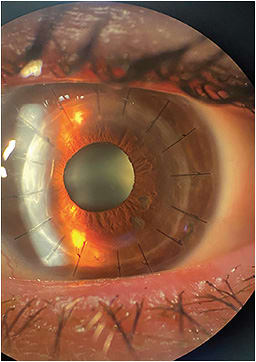
Specfically, this education is comprised of informing patients prior to surgery that they will have a minimum of 10 visits to 12 visits throughout the course of their year of recovery, and that their BCVA will not be obtained until at least one-year post-procedure if everything goes perfectly. They are also made aware of intraoperative complications, such as expulsive hemorrhages and loss of intraocular contents from the open-sky portion of the surgery. These are rare but may happen. Postoperative complications may also occur and include graft rejection, suture complications, endophthalmitis, and steroid-induced glaucoma.
An Irreplaceable Classic
It’s true that other forms of keratoplasty have allowed for quicker recovery times, less intraoperative risk, and VA outcomes equivalent to PK. It’s also true that these procedures have enabled corneal surgeons to tailor therapy to individuals, depending on their anatomical pathology. That said, as the only method of corneal transplantation with long-term success that can treat endothelial dysfunction and stromal opacification and scarring, PK remains relevant. CP
References:
- Park CY, Lee JK, Gore PK, Lim CY, Chuck RS. Keratoplasty in the United States: a 10-year review from 2005 through 2014. Ophthalmology. 2015;122(12):2432-2442.
- Eye Bank Association of America. Statistical report. Eye Bank of Association of America. 2022. Accessed April 23, 2023. https://restoresight.org/members/publications/statistical-report/
- Lim L. Penetrating keratoplasty for keratoconus: visual outcome and success. Ophthalmology. 2000;107(6):1125-1131.
- Watson SL, Tuft SJ, Dart JK. Patterns of rejection after deep lamellar keratoplasty. Ophthalmology. 2006;113(4):556-560.









