Over the past many years, laser vision correction has become a very popular means of eliminating refractive error and becoming glass free. It is known to be very safe and effective, and therefore, has been performed in extremely large numbers around the world. Despite being safe, however, it can sometimes be associated with complications. One of the dreaded complications of laser vision correction is post-LASIK ectasia (PLE). Patients at higher risk of PLE are individuals with thin corneas, high refractive errors, low residual bed thickness, poor biomechanical strength, eye rubbers, patients with altered topography, and underlying form fruste keratoconus.
Presenting as a progressive condition with continuing thinning and protrusion of the cornea, decreased uncorrected and best corrected visual acuity and increased higher order aberrations, this is a condition that needs to be treated before becoming advanced enough to require more invasive surgeries such as deep anterior lamellar keratoplasty or penetrating keratoplasty. PLE can be managed with spectacles and rigid gas permeable contact lenses. These do not treat the underlying condition, however, and therefore the pathology can continue unchecked despite the patient attaining good vision. This may eventually result in the need for other more invasive treatment options such as deep anterior lamellar keratoplasty and penetrating keratoplasty.
Management Options for PLE
Some form of surgical correction is therefore preferred in patients with PLE. It is traditionally treated with corneal cross-linking (CXL) in order to stabilize the cornea. This acts by stiffening the cornea and increasing its biomechanical strength, thereby preventing further protrusion. It may also cause a mild flattening of the cornea. This flattening is however generally not sufficient to give satisfactory refractive results for more advanced cases. Therefore, intra-corneal ring segments (ICRS) such as INTACS and Kerarings have been used in combination with CXL for improving the shape of the cornea. Synthetic ICRS however have the disadvantage of sterile melts and anterior stromal necrosis because of their synthetic nature and interference with corneal nutrition. In addition, they cannot be used for corneas that are thinner or steeper than a certain limit, such as in moderate to advanced keratoconus or post-LASIK ectasia where the need for minimally-invasive techniques is much more required. In addition, they cannot be implanted superficially or along small optic zones, again limiting the amount of effect they can bring. Finally, true customization to each individual patient is difficult to achieve with synthetic segments.
CAIRS and Customized CAIRS
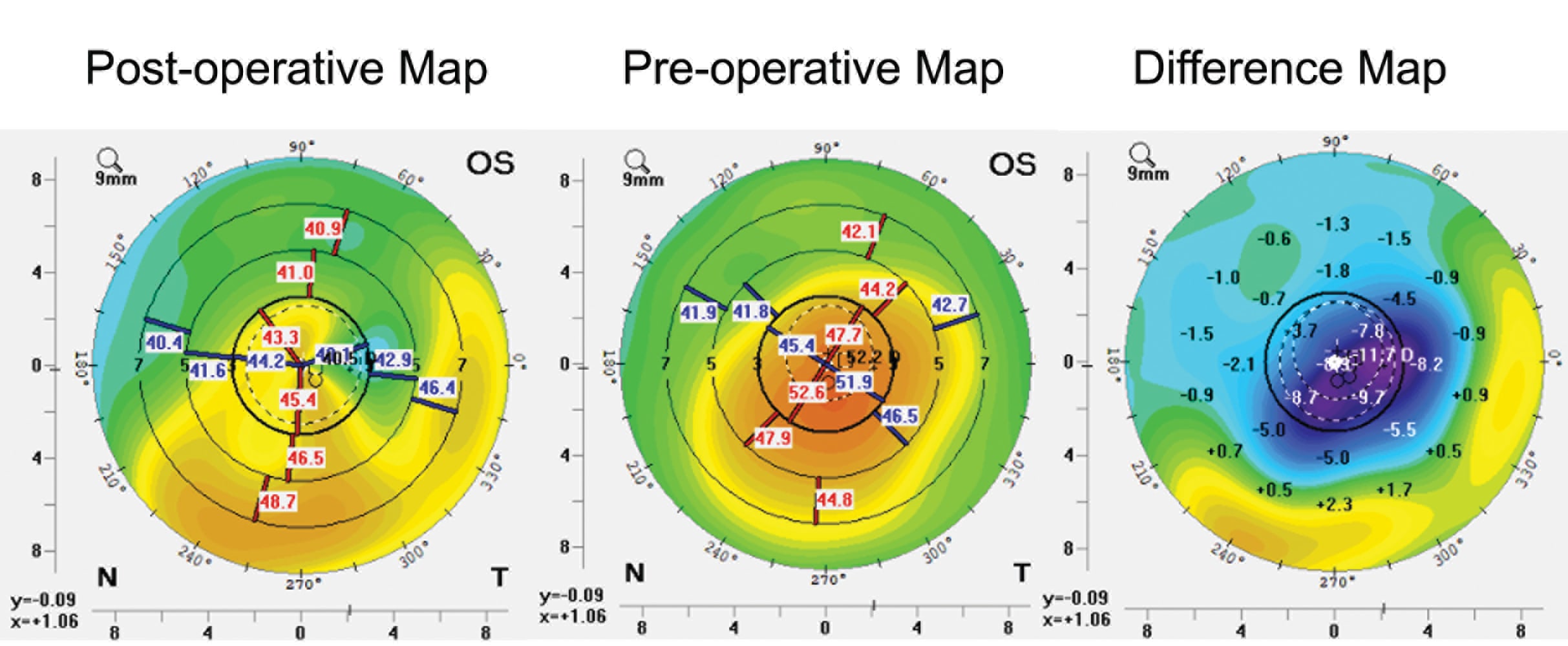
CAIRS were introduced in 2015 (by the author) as a more biocompatible means to treat corneal ectasia.1-3 As the acronym CAIRS clearly indicates, the procedure stands for the use of allogeneic tissue of any source and any type, eg, processed, preserved, pre-cut or segments with shelf life — in short any allogeneic tissue, which are placed as segments into circumferential channels made in the cornea. This brings about a flattening of the cornea and decrease in ectasia because of a volume augmentation effect, an arc shortening effect, and also secondary to epithelial remodeling. Studies from various centers around the world have shown efficacy and safety of CAIRS. My own study has shown a significant improvement in most visual and topographic parameters using CAIRS. Customized CAIRS — which is a technique of further refining the outcomes by personalizing the effect for each individual patient — was also a technique introduced by the author. Personalization brings about the desired amount of regional variation in flattening, thus improving results further. Our published study on customized CAIRS also showed a significant improvement in visual and topographic parameters studied.
We have treated a series of patients with post-LASIK ectasia by using CAIRS combined with CXL with very successful results. Conventionally, CAIRS is inserted into an intrastromal ring channel and can be pushed in using specially designed instruments. However, in patients with PLE, certain precautions need to be taken.
Preoperative Workup
The patient undergoes a detailed slit-lamp evaluation to look for usual signs of keratoconus, as well as to assess the LASIK flap. The flap location, diameter, centration, as well as hinge position are all assessed. Other findings such as scarring, Vogt’s striae, etc., are also looked for. The uncorrected and spectacle corrected distance visual acuity are assessed as is vision with a rigid gas permeable contact lens and pinhole in order to estimate the best potential improvement to vision that is possible. Corneal tomography is performed to assess corneal shape, elevation, curvature and pachymetry together with regional shape and numerical variations in these parameters. Aberrometry is done to assess higher order aberrations. Anterior segment OCT is used to identify the flap margins and to assess the thickness, diameter, edges and profile of the flap. It is also used to assess the cornea in general including the proposed zone of CAIRS implantation, location of the minimum thickness of the cornea and the epithelial mapping. AS-OCT epithelial mapping also helps to confirm the presence of adequate stroma to carry out safe CXL.
Technique
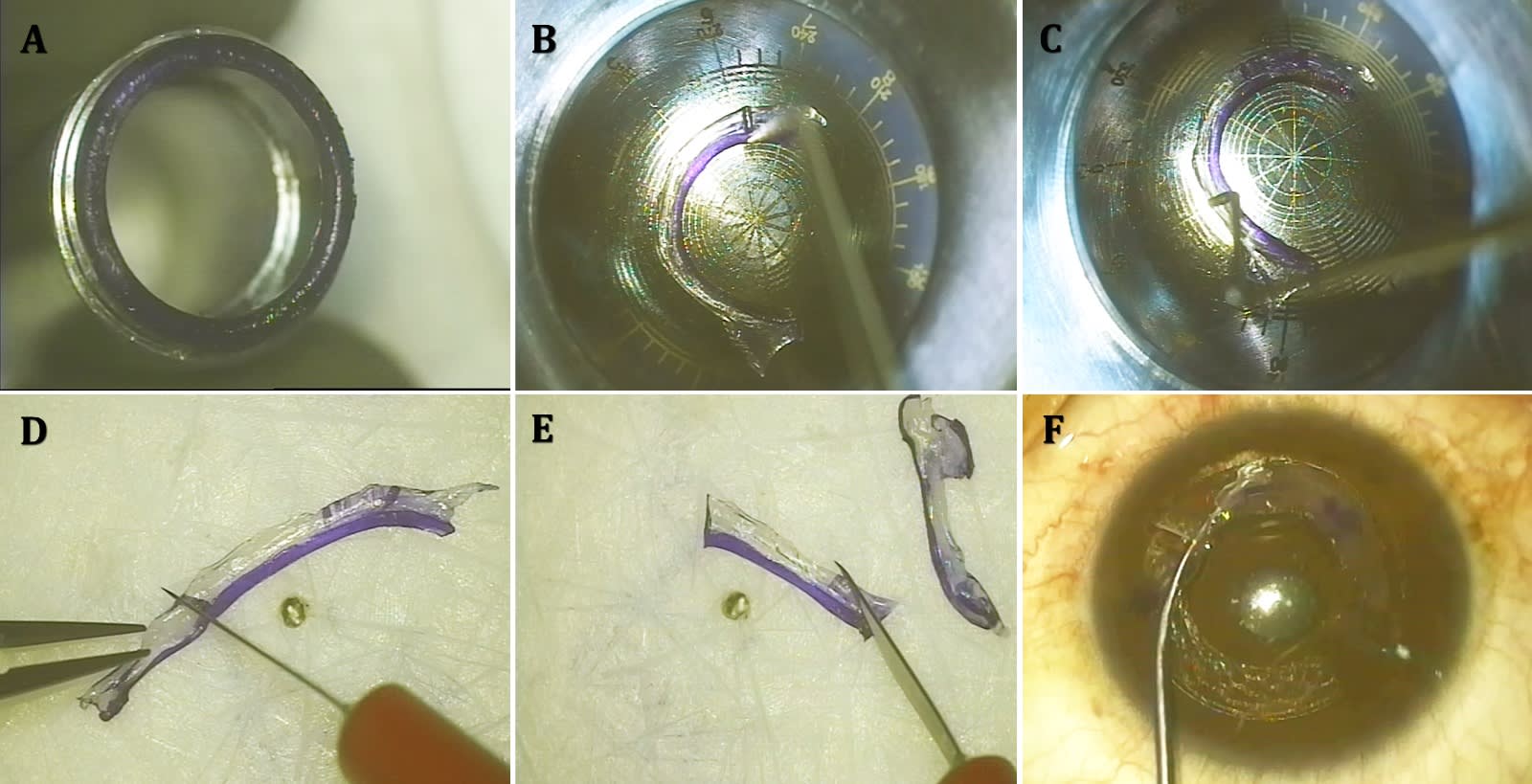
CAIRS Preparation
CAIRS may be made from any source of allogenic tissue. However, the easiest to obtain is the donor corneoscleral rim. The epithelium and endothelium are removed from the rim and a special double-bladed trephine (patented design) is used to cut a circular CAIRS segment. This segment is then placed on the CAIRS customizer (designed by the author), and cut into the custom shape as previously determined by the topographic map, refraction, and other factors. The CAIRS customizer has multiple optic zones as well as radial marks all created true to size. The CAIRS segment is laid along the desired optical zone and the segment is marked as per plan. It is then easily cut into shape using a side-port blade. I have been using custom-shaped CAIRS for many years now, and customized or personalized flattening is tailored to each individual patient. It is therefore not a one-size-fits-all approach or even customization to broad keratoconic phenotypes but customization to each individual patient.
Channel Creation
The depth of implantation of the CAIRS is decided on by taking the thickness of the LASIK flap as measured in the zone of implantation into consideration. Generally, it is preferred to be deeper than the flap by at least 30 to 50 µm which is kept as a safety margin to avoid the CAIRS segments from entering the flap and potentially lifting the flap up. All precautions must be taken to avoid this complication. The coaxially sighted corneal light reflex is then marked on the patient’s cornea and a femtosecond laser channel is created. The length of this channel may be kept a full 360° or extending just beyond the planned segment length. The channel is then opened up using a curved Y-rod or any other curved dissector. The entry incisions cut into both the LASIK flap and the circular channel. It is therefore crucial while opening up the channel to make sure that the inserter enters through the base of the entry incision and not into the plane of the LASIK flap. The Y-rod or channel dissector therefore has to be held facing perpendicular downwards and has to touch the base of the entry incision before changing direction to move circumferentially.
CAIRS Insertion
The prepared CAIRS segment is then inserted carefully through the channel. Care needs to be taken to avoid the segment from accidentally opening up the plane of the LASIK flap. Therefore, the same principle of inserting the segment downward into the entry incision before going forward should be followed. I routinely insert CAIRS segments immediately after cutting and have not found any difficulty with such a technique. The field is kept dry until the leading edge has entered into the tunnel. Further insertion in a dry field with the curved Y rod makes the segment stick to the rod. Therefore, the field is wet with balanced salt solution and the remainder of the now lubricated segment is quickly and easily pushed in. Alternately, the segment may be made stiff by using the Jerky technique described by Awwad et al. In either case, it should be made sure that the segment hits the base of the entry incision before being turned to move further forwards circumferentially. The correct placement of the CAIRS segment can be confirmed by angulating the Y-rod slightly within the tunnel to make sure that the walls of the channel are being felt on either side. If in the LASIK flap plane, the instrument would show a tendency to move freely.
Corneal cross-linking
CAIRS insertion is followed up immediately by CXL. Epi-off CXL is done carefully. Epithelial peeling should be from center to periphery always and not from periphery to center to prevent accidental flap lift. For minimum corneal stromal thickness (after excluding epithelium) above 400 µm, conventional accelerated CXL (10mW/cm2 for 9 minutes) is carried out. For thickness less than 400 µm, contact lens-assisted CXL is used.4 I started this technique in 2012 and have since used only this technique in my large volume center with very good results. CP
References:
1. Jacob S, Patel SR, Agarwal A, Ramalingam A, Saijimol AI, Raj JM. Corneal allogenic intrastromal ring segments (CAIRS) combined with corneal cross-linking for keratoconus. J Refract Surg. 2018;34(5):296-303.
2. Jacob S, Agarwal A, Awwad ST, Mazzotta C, Parashar P, Jambulingam S. Customized corneal allogenic intrastromal ring segments (CAIRS) for keratoconus with decentered asymmetric cone. Indian J Ophthalmol. 2023;71(12):3723-3729.
3. Jacob S, Agarwal A, Awwad S, Parker J, Mimouni M, Sambath J. Bowman layer marking for correct placement of corneal allogeneic intrastromal ring segments. Cornea. 2024;43(3):398-401.
4. Srivatsa S, Jacob S, Agarwal A. Contact lens assisted corneal cross linking in thin ectatic corneas - a review. Indian J Ophthalmol. 2020;68(12):2773-2778.